Abdominal and Pelvic Radiography
Objectives:
- List all the steps to perform abdominal and pelvic imaging
- Identify common abdominal and pelvic pathologies
- Understand the concept of magnification and know how to apply it
- Ensure that physicians’ imaging orders are carried out correctly and at the right times
- Apply appropriate patient shielding to reduce the patient dose
Description:
For many years, X-rays were used for imaging different organs of the human body using different methods of positioning and variable technical factors. This course helps radiologic technologists understand the different steps to obtain accurate, consistent images according to body type, the abdominopelvic anatomy, and the pathologies that may affect the quality of the image.
Knowing that there are four body habitus and that anatomy differs from one type to another, this course presents the technical modifications that radiographers shall apply to avoid any unexpected error caused by the anatomy of the patient. In addition, it describes the abdominopelvic image details that shall be clarified, allowing physicians to diagnose the cases of different patients.
This course also describes the best patient position to reduce magnification, as well as the high voltage and the exposure time product required to obtain better images of the abdomen and pelvis. Finally, the course defines the stochastic and non-stochastic effects of radiation, helps to organize the procedures to carry out physician orders, and describes how to use shielding appropriately during imaging to reduce the patient’s exposure to radiation. This article is accredited by the ASRT for 1.75 Category A CE Credits.
Abdominal and pelvic radiography is helpful in the detection of many pathologies. Therefore, radiographers must know the clinical indications for abdominal and pelvic radiography, and the patient anatomy. Besides, they should as well be able to distinguish certain pathologies in order to notify the radiologist when a study needs to be read immediately.
The purpose of this article is to introduce users to the use of X-ray for abdominal and pelvic imaging. It also helps radiographic technologists to determine the best position of the patient according to his body habitus. This article will as well present all the abdominal and pelvic pathologies requiring radiography. It also highlights the concept of image magnification in addition to the quality control program and radiation protection practices.
By reviewing positioning, techniques, anatomy, shielding, and evaluation criteria for each abdominal and pelvic image, this article will help each radiologic technologist in producing consistent optimal images.
X-rays are the oldest and most frequently used form of medical imaging. X-ray uses a very small dose of ionizing radiation to produce images of the body’s internal structures. They are often used to help diagnosed fractured bones, look for injury or infection, and to locate foreign objects in soft tissue such as abdominal and pelvis tissues.
Furthermore, radiographers, also known as radiologic technologists, are certified technicians who capture images of organs, bone, and tissue for patient diagnosis. They are equipped with the technological skills to handle imaging equipment as well as the interpersonal skills necessary for patient care.
Radiologic technologists are important members of the healthcare team, and most of the time, physicians rely on them to produce consistently high quality radiographic images, and because as we all know pathologies can be misrepresented if the proper techniques to acquire the images were not used correctly.
Unfortunately, in many hospitals and clinics, the radiographers are obliged to irradiate the patient multiple times to acquire the results that physicians want. Therefore, to avoid this unnecessary radiation, we ask you to complete this article that will help you gain knowledge to acquire optimal images regardless of factors that are inherent in the patient.
Besides, body type affects the location and the size of the organs in the abdominal and pelvic cavities, which in turn affects positioning and exposure factors.
This article will review the indications for abdominopelvic radiography, and the guidelines to perform a proper abdominal and pelvic imaging procedure, including evaluation criteria.

This article will also provide information on patient positioning, abdominal and pelvic pathologies, magnification, and guaranteeing that physicians’ imaging orders are carried out accurately and at the correct time. It will also help you understand how to protect patients from unnecessary radiation through appropriate shielding.
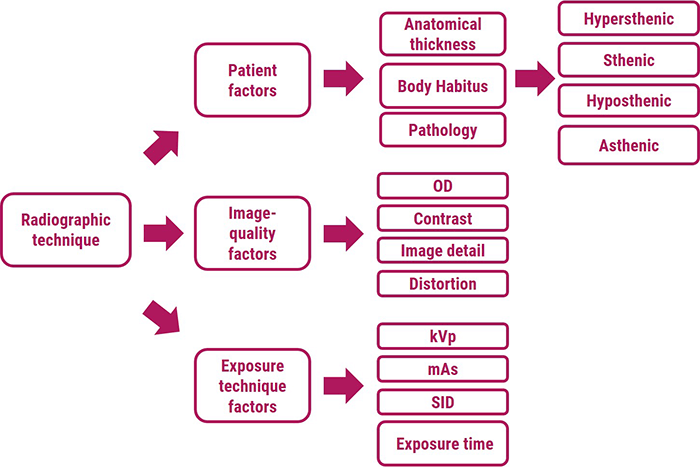
As shown in this diagram, radiographic technique is a combination of different factors used to expose a well-defined anatomical part to produce a high-quality radiographic image.
- Patient factors
- Image-quality factors
- And exposure technique factors
Patient factors include anatomical thickness, body composition, and any pathology that is present. Radiographers recognize sthenic, asthenic, hyposthenic, and hypersthenic body habitus types as a way to determine body composition and thus to select proper radiographic technique. Pathology in the body may be destructive and therefore radiolucent, which requires a reduction in technique, or constructive and therefore radiopaque, which requires an increase in technique.
Image-quality factors include Optical Density (OD), contrast, image detail, and distortion. Optical density, which means blackening of the radiograph, is defined as the log of the incident light over the transmitted light. The Contrast is the difference in the optical density between adjacent anatomical structures. Whereas high kVp produces low-contrast images, low kVp produces high-contrast images. Image detail is the sharpness of the image on the radiograph. To produce the sharpest image detail, the smallest focal Spot, the longest SID (Source – image distance), and the least OID should be used. Distortion shape on the radiograph refers to misrepresentation of object size or shape on the radiograph.
Radiographic exposure factors (kVp, mAs, and SID) are manipulated by radiologic technologists to produce high-quality radiographs. Exposure factors influence radiographic quantity (number of X-ray) and quality number (penetrability of the X-rays). Therefore, proper selection of exposure factors optimizes the spatial contrast resolution of the image.
Moreover, the two technique charts used most commonly by radiographers to produce consistently high-quality radiographs are the fixed-kVp and the high-kVp.
- The fixed-kVp chart uses approximately 60 kVp for extremity radiography and approximately 80kVp for the examinations of the abdomen and pelvis parts of the body
- The high-kVp chart is used for barium studies and chest radiographs with kVp from 120 to 135 kVp
Even with AEC (Automatic Exposure Control), radiographic exposure chart is required. APR (Anatomical Programmed Radiography) uses microprocessor technology to program the technique chart into the control unit. The radiographer selects an anatomical display of the body part, then the microprocessor selects automatically the appropriate kVp and mAs settings.
Before we go any further in this discussion, we need first to well understand the abdominal and pelvic anatomy.
First, we shall know where is located the abdominal and pelvic cavity. The abdominal cavity is a large cavity found in the torso between thoracic pelvic cavities. It is separated from the thoracic cavity by the diaphragm.
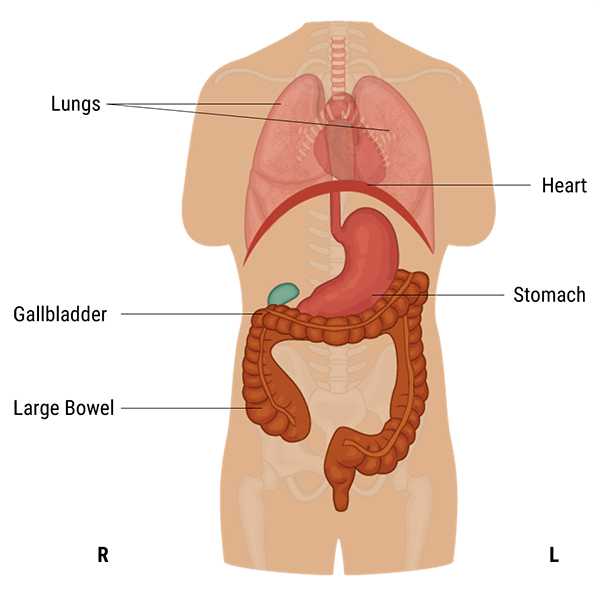
A protective layer called the peritoneum, which plays a role in supporting organs, immunity, and fat storage, lines the abdominal cavity. As shown in this diagram, there is no overlapping partition between the pelvic and abdominal cavities.
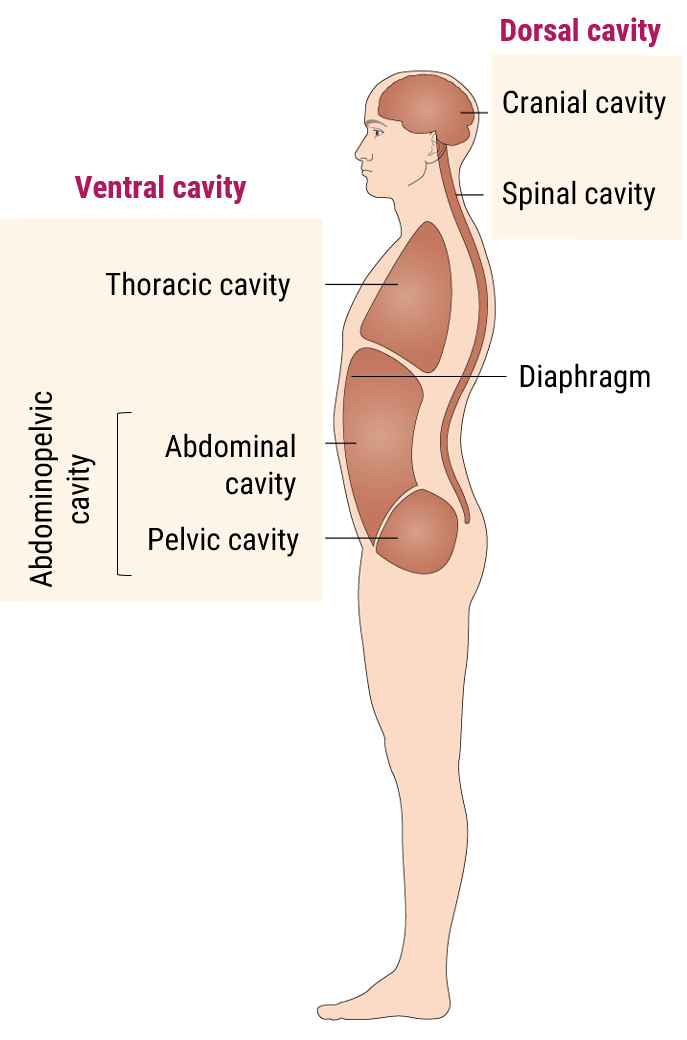
Now let’s talk about the anatomy of the abdominal cavity and have a summary of the function of each organ.
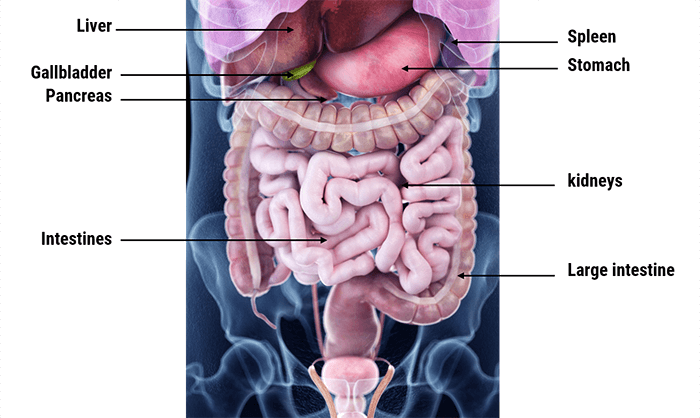
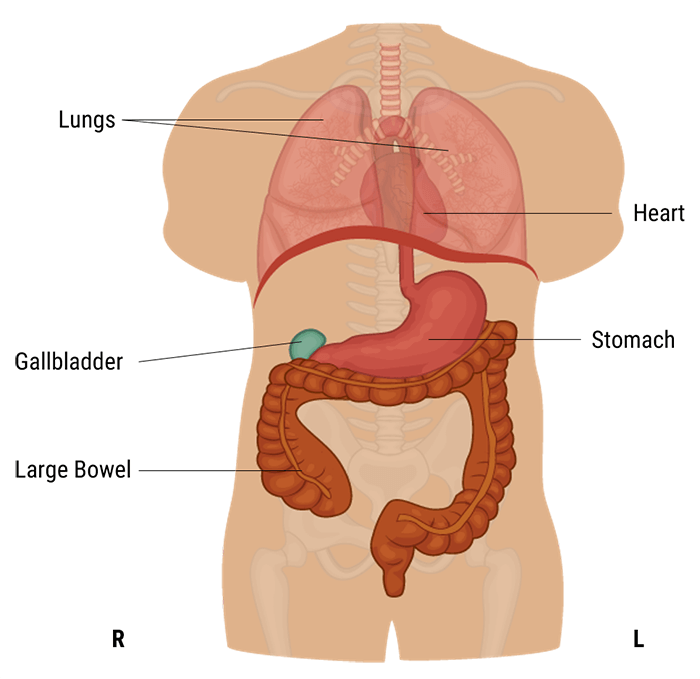
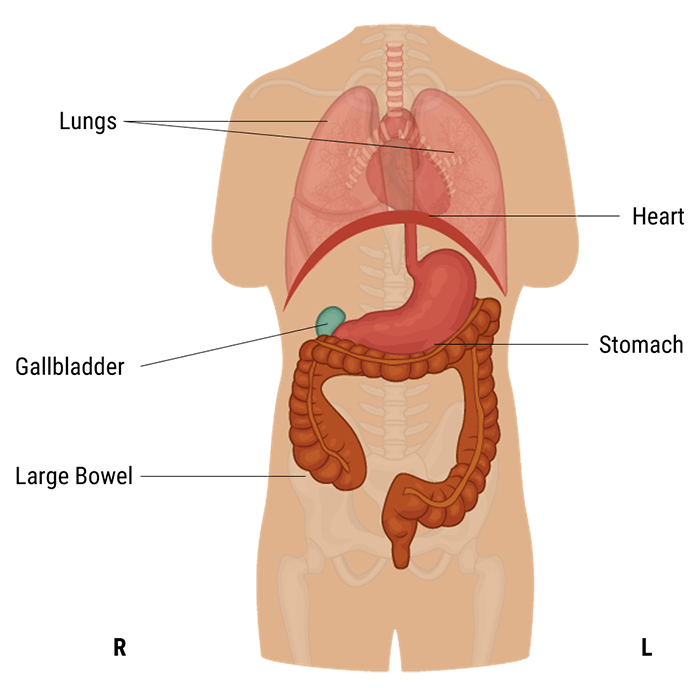
The abdominal cavity is the largest body cavity in humans, it is lined by a thin, serous membrane called the peritoneum and contains different vital organs such as the liver, gallbladder, stomach, spleen, pancreas, kidneys, ureters, intestines, and the arterial and venous systems.
The stomach is a thick-walled digestive organ found on the left side of the abdomen. It is followed by the first portion of the small intestine, called the duodenum.
The Liver is the largest organ in the abdomen. It is located on the upper right side of it, right under the diaphragm. It has two lobes that are separated by a ligament. It plays a crucial role in our bodies as it maintains normal blood glucose levels, produces bile, and detoxifies the blood.
The Gall bladder is found below the liver and is connected to it. It stores and concentrates bile that is sent to the duodenum when needed for fat digestion and absorption.
The spleen is part of the immune system. Its functions include taking part in the production of white blood cells, storing platelets, and destroying dead red blood cells and harmful substances.
The Pancreas is a part of the digestive system, it produces important digestive enzymes, as well as insulin and glucagon, which are crucial for the metabolism of carbohydrates in our bodies.
The small intestine is found between the stomach and large intestine and is made up of three parts: the duodenum, jejunum, and ileum. It is a long, tube-shaped digestive organ, where digestion and absorption of nutrients take place.
The large intestine is the organ to which undigested material is sent. It is U-shaped and is made up of the cecum, colon, rectum, canal, and appendix. Absorption of water and electrolytes and the formation of feces all occur here.
The two kidneys are found on either side of the abdomen. They play an essential role in the body, because they ensure the detoxification of the blood, the creation of urine, and the maintenance of water and acid balance in the body. Attached to each kidney are tubes, called the ureters, which connect them to the urinary bladder. In addition to the kidneys’ functions, the adrenal glands found on the kidneys produce important hormones, such as norepinephrine and ADH.
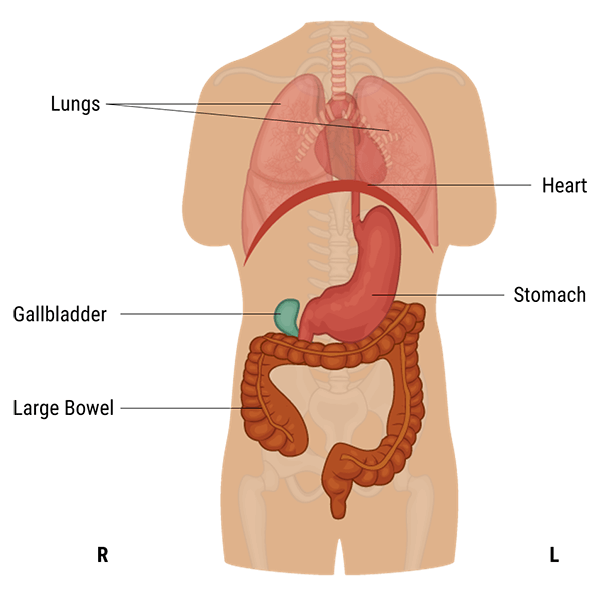
The pelvic cavity is a body cavity that is bounded by the bones of the pelvis. It contains primarily the reproductive organs, the urinary bladder, the pelvic colon, and the rectum. In the female, the uterus and vagina occupy the interval between these viscera.
- The rectum is placed at the back of the pelvis, in the curve of the sacrum and coccyx
- The bladder is in front, behind the pubic symphysis
- The internal iliac artery
- The median sacral artery
- The ovarian artery
- The sacral plexus
- The splanchnic nerves
- And the femoral nerve
These structures coexist in a crowded space, and disorders of one pelvic component may impact upon another; for example, constipation may overload the rectum and compress the urinary bladder, or childbirth might damage the pudendal nerves and lead to anal weakness.
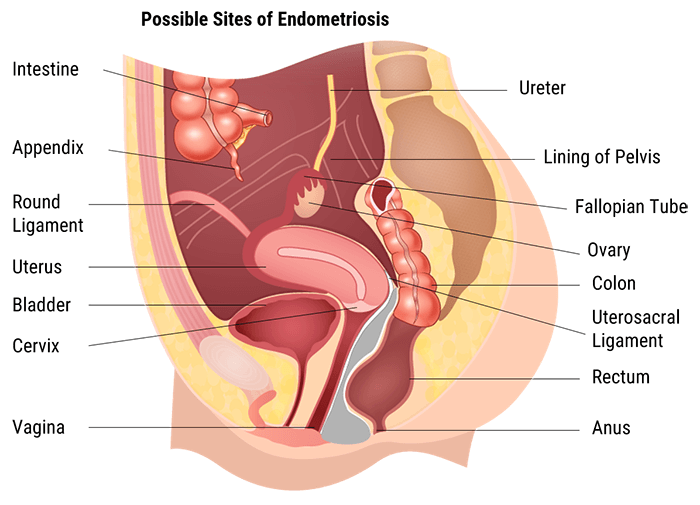
Each radiographer shall obtain a relevant medical history from a patient regarding the area that requires imaging before starting the exam. The information must be decoded and then sent correctly to the radiologist. Patients often refer to any region of their abdominopelvic cavity as their “stomach”. However, it is possible to determine the quadrant or the region of interest by asking the patient to point to the area of interest.
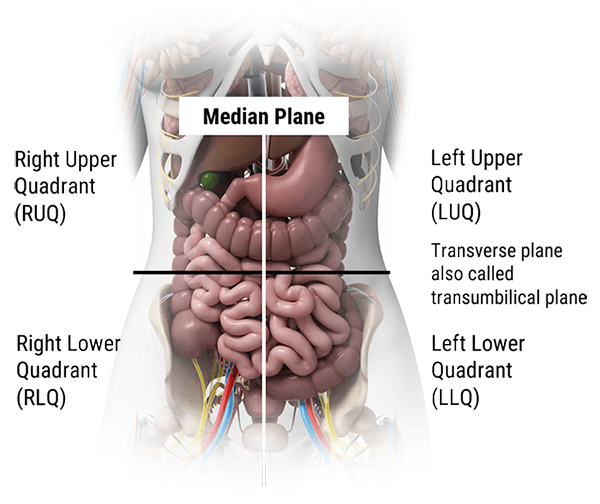
In this section we will explain how the abdominopelvic cavity is divided into 4 quadrants or 9 regions.
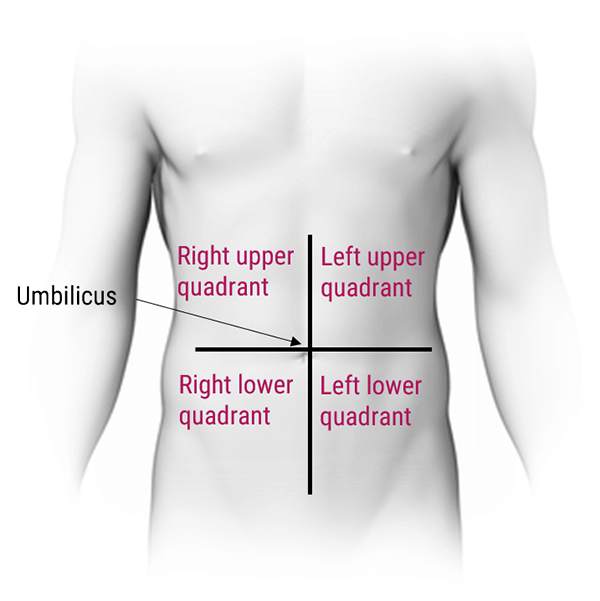
As shown in this diagram, the abdominal cavity has been divided into four quadrants: the right upper quadrant, the left upper quadrant, the right lower quadrant, and the left lower quadrant. These quadrants have different abdominal and pelvic organ systems. For example, the right upper quadrant contains the liver, gallbladder, and right colic flexure, whereas the right lower quadrant contains the appendix, terminal ileum, and right ovary in females.
The 4 quadrants are divided by 2 planes: the midsagittal plane and the horizontal plane at the level of the umbilicus.
- The navel also called belly button, the point at which the two planes cross, is the landmark you’ll use to visualize these quadrants while doing assessments
- The terms “left/right” and “upper/lower” are always from the perspective of the anatomical position, not your perspective. Be careful not to mix up your right and left regions, as this is where most students make a mistake!
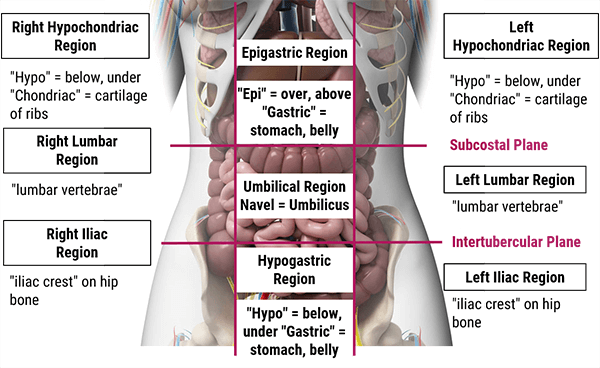
The abdominal cavity can be divided into nine different regions using 4 planes, where every organ doesn’t necessarily occupy only one. This division helps with the diagnosis, based on the place where the patient is experiencing abdominal pain.
The nine regions are smaller than the four abdominopelvic quadrants and include: the right hypochondriac, right lumbar, right illiac, epigastric, umbilical, hypogastric (or pubic), left hypochondriac, left lumbar, and left illiac divisions.
- In the Right Hypochondriac region, you will find organs such as the liver, gallbladder, right kidney, and portions of the small and large intestine
- The epigastric region contains portions of the liver, as well as the stomach, pancreas, duodenum, spleen, and adrenal glands
- Whereas the left hypochondriac region contains the spleen, large/small intestines, left kidney, pancreas, stomach, and tip of the liver
- In the right lumbar region, you will mainly find portions of the ascending colon, small intestine, and right kidney
- In the umbilical region, you’ll find the duodenum, the small intestine, as well as the transverse colon
- Whereas in the left lumbar region, you’ll find parts of the descending colon, small intestine, and left kidney
- The right iliac region contains the appendix, cecum, ascending colon, and small intestine
- The hypogastric region contains the bladder, portions of the sigmoid colon, small intestine, and reproductive organs
- And finally, the left iliac region where you will find parts of the sigmoid colon, descending colon and small intestine
Now, let’s move to one of the most important topics covered in this article.
In this section, we will discuss the different body types and characteristics to understand how they affect the image quality in radiography.
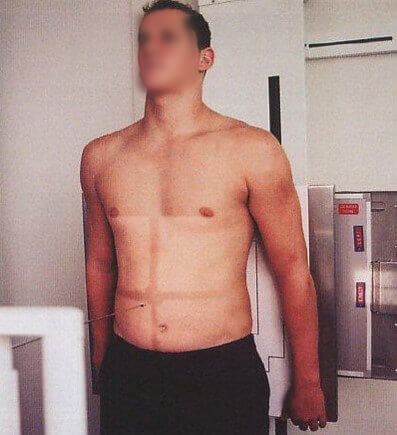
As we know, every patient has a different body type. Body habitus is not an indication of disease or other abnormality, it describes the physical characteristics of an individual and includes different considerations such as physique, general bearing, and body build.
- Hypersthenic 5% of adults
- Sthenic 50% of adults
- Hyposthenic 35% of adults
- Asthenic 10% of adults
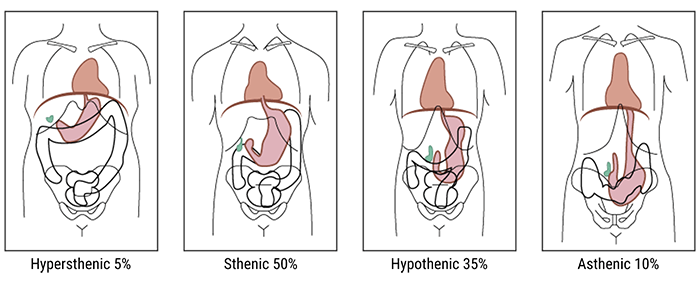
Hypersthenic
The first body type to discuss is the “hypersthenic” one.
A hypersthenic person is a very muscular, thick-set individual, with a broad bony chest and high diaphragm. In this body type, the stomach tends to lie transversely and the gall-bladder horizontally high in the abdomen, well away from the midline. The transverse colon is also high, as well as the heart and the lungs.
Sthenic
A sthenic person is a muscular, thick-set individual similar to hypersthenic but not quite as broad in relation to height. The stomach and gall-bladder lie more vertically and the transverse colon curves lower.
Asthenic
Whereas, asthenic individuals have a long, thin, and lean chest with the diaphragm, stomach, gall-bladder, and transverse colon situated lower down than hypersthenic and sthenic types. In the erect position, the stomach and transverse colon descend into the pelvis.
The radiographer has to take all these variations into account while positioning the patient for imaging.
Hyposthenic
Finally, hyposthenic individuals are similar to those of the asthenic type but stomach, intestines, and gallbladder are situated higher in the abdomen. They are characterized by a long, shallow thorax, a long thoracic cavity, a long, narrow abdominal cavity, and a slender build.
Hyposthenic and sthenic patients have very similar organ placement. Little or no manipulation of the grid, milliamperage, source-to-image distance (SID), or kilovolts peak are needed because these technical factors are almost interchangeable for hyposthenic and sthenic patients.
On the other hand, the radiographer has to increase these technical factors for hypersthenic patients and to decrease them for asthenic patients to improve the image quality. Let’s see the difference in the image clarity below.
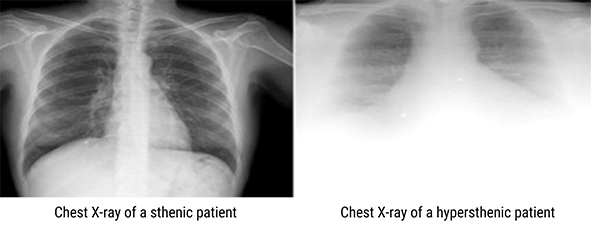
This image shows a chest X-ray of a sthenic and hypersthenic patients.
As you can see, the image on the right needs a large adjustment of technical factors to produce an image of optimal density. However, the image on the left shows X-ray penetration of the abdominal cavity below the diaphragm with clearly visible lower ribs and spinal structures.
Please keep in mind that on some hypersthenic patients, an image of optical density may not be achievable.

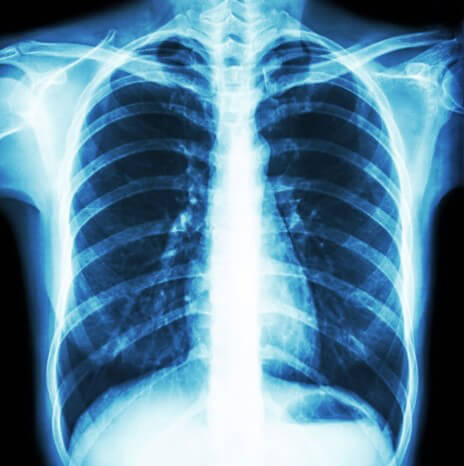
Moreover, this image is an example of an abdominopelvic X-ray on a hypersthenic patient. It shows poor penetration and poor optical density.

And finally, we can see here an example of an abdominopelvic X-ray showing proper optical density, penetration, and organ size, shape, and alignment.
Because the placement and the size of the organs significantly affect the positioning and the selection of exposure factors, let’s discuss the different types of abdominopelvic radiography, and how to improve the quality of images according to the anatomy of interest and the body habitus of the patient.
Indications for Abdominopelvic Radiography
Abdominopelvic radiography is useful in the diagnosis of different pathologies. Before the advent of computed tomography (CT) imaging, it was a primary means of investigating gastrointestinal pathology.
Indications for abdominopelvic radiography include abdominal distension or chronic pain, acute abdominal or pelvic pain, suspected foreign body, abdominal trauma, chronic abdominal pain with acute exacerbation, known or suspected renal calculi, and to localize an enteric tube or other device.
Acute Abdominal Series
The acute abdominal series is a common set of abdominal radiographs acquired to evaluate bowel gas. For patients who are unable to stand or sit upright, projections used to complement the supine anteroposterior (AP) projection include an upright AP or a lateral decubitus projection. Often an upright posteroanterior (PA) projection of the chest will be ordered in conjunction with an upright AP abdomen and supine AP abdomen. This is known as an acute abdomen series at some facilities.
Shall we include the chest film in the AP abdomen image? Yes, the chest film shall be included for many reasons. The main reason is that conditions such as pneumonia or pleural effusions can present as abdominal pain.
The main reason is that conditions such as pneumonia or pleural effusions can present as abdominal pain. The ordering physician must be specific when ordering abdominal projections, and the radiographer must be precise when imaging the patient and shall perform only the projections that were ordered.
Confusing an abdominal series with an acute abdominal series is an easy error to make. The PA chest X-ray will mainly show the lungs, heart, diaphragm, mediastinum, and soft tissues. Whereas, an AP projection of the abdomen will show the shape and the size of the liver, spleen, and kidneys. Intra-abdominal calcifications can also be seen on an AP projection.
However, intestinal perforations, air fluid levels and obstructions are detected on an upright abdomen when compared to a supine abdominal X-ray.
When checking the acquired images, the radiologist will look at the abdominal gas pattern, the renal shadows, the edge of the liver and spleen, the preperitoneal fat lines. He will look as well for abnormal calcifications, and review the skeletal structures to determine if abnormal pathology exists.
To obtain proper optical density the radiographer must determine many technical factors based on patient thickness and density. For example, air is less dense and would require a decrease in technical factors to obtain a proper optical density.
PA Erect Chest X-Ray
What are the PA Erect Chest X-ray characteristics?
For a proper PA erect chest X-ray, the patient shall stand at 72in and face the wall bucky with his body weight equally distributed between both feet. The technologist shall adjust the height of the wall bucky so the image receptor is 3.8 to 5 cm above the patient’s relaxed shoulders.
As we can see, the midsagittal plane of the patient’s body is centered to the midline of the image receptor entering the level of T7.
Ask the patient to extend his or her chin upward, place the back of the hands on his/her hips, and roll the shoulders and arms forward. Finally, place a lead shield between the X-ray tube and the patient, and instruct the patient to control his breathing during irradiation.

How to evaluate the image obtained?
- The entire lung fields shall be visible from the apices down to the lateral costophrenic angles and three posterior ribs should be seen above the superior aspect of the clavicle
- The chin should not be superimposing any structures, and sternoclavicular joints are equal distant apart
- The clavicle is in the same horizontal plane, 10 posterior ribs are visualized above the diaphragm and the trachea in the midline
- The ribs and thoracic cage are seen only faintly over the heart and clear vascular markings of the lungs should be visible
- The annotations should be present on the image
AP Erect Abdominal X-Ray
Now let’s discuss the characteristics of the AP Erect Abdominal X-ray.
The patient should be standing with his or her back to the wall bucky at 48 in from the source with his weight equally distributed on both feet.
The radiographer should center the midsagittal plane of the body 2 inches (5 cm) above the iliac crest and use the Automatic exposure control with all detectors to improve the image clarity.
Finally, to protect the organs at risk, use gonadal shielding to cover the lower half of the pelvis.
Do not forget to ask the patient to suspend respiration after exhaling, so the abdominal organs are not compressed.
- The diaphragm must be shown on the AP erect and the entire diaphragm must be seen without motion
- Lateral abdominal wall should be included
- No rotation at the abdomen level with symmetry of the: Ribs (superior), Iliac crests (middle), and Obturator foramen (inferior)
- No blurring of the bowel gas due to respiratory motion and anatomy should not be obscured
- Add image annotation
- Anatomy shall not be obscured by shielding or marker placement
AP Erect Abdominal X-Ray
Moving forward to the AP Supine Abdominal X-Ray.
As we mentioned earlier, the supine abdomen X-ray is referred to as the KUB because it includes the kidneys, ureters, and bladder.
The patient should be supine on the table bucky at 48in from the source with knees slightly flexed and the midsaggital plane of the patient’s body centered to the midline of the table bucky. For male patients, the radiographers shall cover appropriately the lower part of the pelvis with gonadal shielding.
Please note that shielding cannot be used in female patients, as it will directly obscure the anatomy.
Finally, ask the patient to suspend respiration after exhaling to avoid abdominal compression.
- Entire diaphragm must be seen without motion
- Lateral abdominal wall should be included
- No blurring of the bowel gas due to respiratory motion
- Soft tissue grey tones demonstrating: Lateral abdominal wall if possible, Psoas muscles, Inferior ribs, Diaphragm, Transverse process of lumbar vertebrae, and Superior ilia
- Annotations must be clear on the image
- Anatomy should not be obscured by shielding

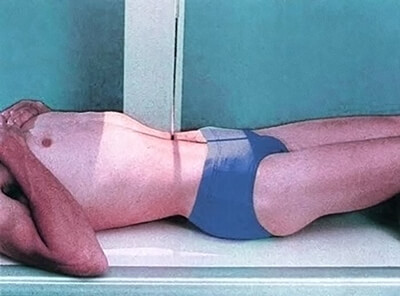
AP Decubitus Abdominal X-Ray
Now, for the AP Decubitus Abdominal X-ray, as shown here, the patient is in supine lying on his left side with knees slightly flexed and arms overhead at 48in from the X-ray tube. The midsagittal plane of the body shall be centered to the midline of the image receptor.
Center the central ray to the midsagittal plane at the level of the iliac crest and shield appropriately with gonadal shielding over the testes in males. Again no shielding is applied for female patients as it will directly obscure the anatomy.
Finally, ask the patient to suspend respiration after exhaling to avoid abdominal compression.

- The elevated lateral abdominal wall is included on the image to detect any free intraperitoneal gas
- There should be no blurring of the bowel gas due to respiratory motion
- Soft tissue grey tones demonstrating lateral abdominal wall if possible, psoas muscles, inferior ribs, diaphragm, transverse process of lumbar vertebrae, and superior ilia
- And finally, the anatomy should not be obscured by shielding or marker placement

AP Pelvis
Finally, for AP pelvis radiography, the patient should be supine.
Radiographers shall center the midsaggital plane of the patient’s body to the midline of the image receptor. The central ray should be centered to the midsagittal plane at the level of the iliac crest.
Don’t forget to shield appropriately with gonadal shielding over the testes in males. Again no shielding is applied for female patients as it will directly obscure the anatomy.

- Entirety of the bony pelvis is imaged from superior of the iliac crest to the proximal shaft of the femur
- Obturator foramina appear equal
- Sacrum coccyx is aligned with the pubic symphysis depicting lack of rotation
- Lesser trochanters demonstrated on the medial border of the femora
- Iliac wings present an equal concavity
- Greater trochanters of the proximal femur are in profile
- Anatomy should not be obscured by marker placement or shielding and should be marked correctly

Comparison of the Equivalent Dose
Equivalent dose is an important consideration when ordering any imaging investigation. Therefore let’s compare the equivalent dose of different radiographs.
An abdominal radiograph in an average patient produces a radiation dose of approximately 1.5 mSv. This is equivalent to seventy-five chest radiographs (0.02 mSv) or approximately one sixth of the dose produced by a standard CT of the abdomen (9–10mSv). The abdominal radiograph, like all ionizing radiation procedures, should therefore be used appropriately.
Radiologic technologists shall be able to distinguish certain abdominal and pelvic pathologies to notify the radiologist when a study needs to be read immediately.
This section will cover the following pathologies: small-bowel obstruction, adynamic Ileus, pelvic kidney from transplant, renal calculus, pneumoperitoneum and foreign Body evaluation.
Small-Bowel Obstruction
What is Small bowel obstruction?
Small-Bowel obstruction is a common clinical condition that occurs secondary to mechanical or functional obstruction of the small bowel, preventing normal transit of its contents. It is a partial or complete blockage of the small intestine, which is a part of the digestive system. It is a frequent cause of hospitalization and surgical consultation and usually presents as acute abdominal pain with nausea, vomiting, bloating, and diarrhea.
Small bowel obstruction can be caused by adhesions, hernia and inflammatory bowel disorders.

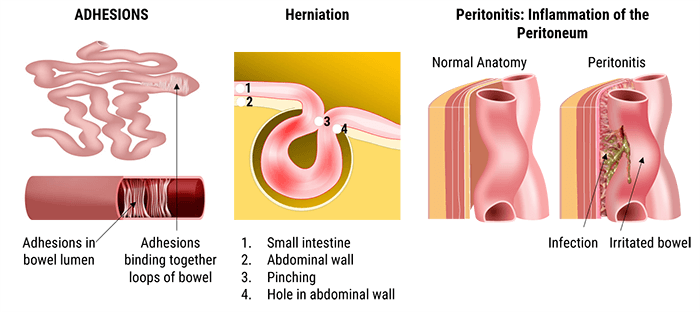
Abdominal adhesions are bands of scar-like tissue that may form between abdominal tissues and organs. A hernia is an abnormal exit of the bowel, through the wall of the cavity in which it normally resides.
Peritonitis is an inflammation of the peritoneum which lines the abdominal cavity and covers the abdominal organs. According to many studies, small bowel obstructions are most often due to adhesions and hernias while large bowel obstructions are most often due to tumors and volvulus.
In general, the abdominal X-ray is used to diagnose small-bowel obstructions; however, ultrasound or MRI may be used for children and pregnant women.
A dynamic Ileus
What is a dynamic ileus?
A dynamic ileus is a common disorder of intestinal motor activity. It is the failure of passage of fluid and gas through the small bowel and colon.
- Drugs
- Poor nutritional intake
- Large amounts of narcotic pain medications
- Myocardial infarction or congestive heart failure
- Head injury or neurosurgery
- Intra-abdominal inflammation and peritonitis
- Retroperitoneal hematoma
- And acute mesenteric ischemia: ileus limited to a vascular territory
The cause of ileus is thought to be complex and multifactorial, involving bowel inflammation, inhibitory neural reflexes, and neurohormonal peptides.
Moreover, the lack of oral intake, disrupts the normal coordinated propulsive motor activity of the intestines, and causes severe constipation.
In general, surgeons expect a certain degree of postoperative ileus, as a physiological response to abdominal, and non-abdominal surgery.
- 0 to 24 hours for small intestine
- 24 to 48 hours for stomach
- And 48 to 72 hours for Colon
Pelvic Kidney from Transplant
You have certainly heard about Kidney transplant, let’s enhance your information by answering the following questions. What does kidney transplant mean? And why do people need kidney transplants?
Ectopic pelvic kidney is a relatively rare congenital anomaly in which the kidney fails to ascend to its lumbar position during embryonic development. Kidneys for transplantation may come from cadaveric donors or living donors. Essentially, the donor kidney must be anatomically and functionally suitable for transplantation, and the donor must be in good medical and psychological health and left with a good renal function from the remaining kidney.
The location of an ectopic kidney can be pelvic, lumbar, abdominal, and thoracic or crossed fused. Ectopic pelvic kidney slightly occurs more on the left side with predominance in male subjects. The kidney is then attached to the ureter on the side of the implantation. The diseased kidneys are left in place and will be visible on the X-ray. And thus a third kidney will be visible in the pelvis.
Renal Calculus
Calculus is a stone found inside the gallbladder, intestine, bladder, kidney, or lower down in the urinary tract. The most known are the renal calculus called renal stones or calculi. They are composed of calcium crystals that form in the kidneys. Renal calculus are a common cause of blood in the urine and pain in the abdomen, flank, and occur in 1 in 20 people at some time in their life. The development of the stones is related to decreased urine volume or increased excretion of stone-forming components such as calcium, oxalate, urate, cystine, xanthine, and phosphate.
CT of the abdomen and pelvis is the preferred diagnostic imaging study for the initial assessment of suspected renal calculi. A KUB radiograph is recommended for follow-up to determine the progression of the calculi due to the reduced amount of radiation with plain film radiographs in comparison with computed tomography.
Most kidney stones will pass through the ureter to the bladder on their own with time. Treatment includes pain-control medications, and in some cases, medications to facilitate the passage of urine.
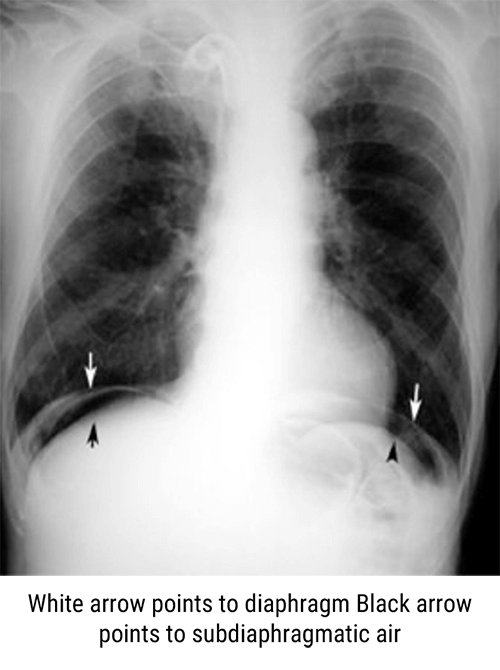
Pneumoperitoneum
The peritoneum is the serous membrane forming the lining of the abdominal cavity. It covers most of the intra-abdominal organs, and is composed of a layer of mesothelium supported by a thin layer of connective tissue.
Pneumoperitoneum describes gas within the peritoneal cavity, often due to critical illness. There are numerous causes of pneumoperitoneum. These include ischemic bowel, appendicitis, diverticulitis, malignancy, inflammatory bowel disease, necrotizing enterocolitis, and bowel obstructions.
The most common cause of pneumoperitoneum is from the disruption of the wall of a hollow viscus. It is important to know that causes for pneumoperitoneum in adults differ from those in children.
- Rated hollow viscus
- Peptic ulcer disease
- Ischemic bowel
- Bowel obstruction
- Necrotizing enterocolitis
- Appendicitis
- Diverticulitis
- And malignancy
- Perforated hollow viscus including necrotizing enterocolitis (NEC), meconium ileus in cystic fibrosis, hirschsprung disease and intestinal atresia
- And Iatrogenic including intubation or mechanical ventilation, rectal thermometer and enema
Foreign Body Evaluation
Finally, the evaluation and treatment of a foreign body will depend on the type of the foreign body and how it was introduced. If it was swallowed, patient may undergo a direct examination of his throat and esophagus or an X-ray examination. If it is lodged in a soft tissue, patient may undergo an ultrasound, x-ray or CT scan to locate and remove the object.
In adult women, considerations include tampons, condoms, menstrual cups, and items used for sexual gratification. Elderly patients are at increased risk for retained medical devices such as pessaries. Patient populations such as prisoners and drug traffickers may use the vaginal canal and uterus to hide illicit substances.
Rectal foreign bodies can also be difficult to image. A professional behavior must be maintained at all times and Health Insurance Portability and Accountability Act (HIPAA) guidelines must be followed. In most instances the patient is often embarrassed by the situation, and maintaining a professional stance will reassure the patient and not cause any added discomfort.
Perform only the examinations requested by the physician. Keep in mind that an upright abdomen should be performed to include the diaphragm for the evaluation of intestinal perforation.
Now, let’s highlight some practical tips that can help the technologist in minimizing the exposure dose, and enhancing the image quality.
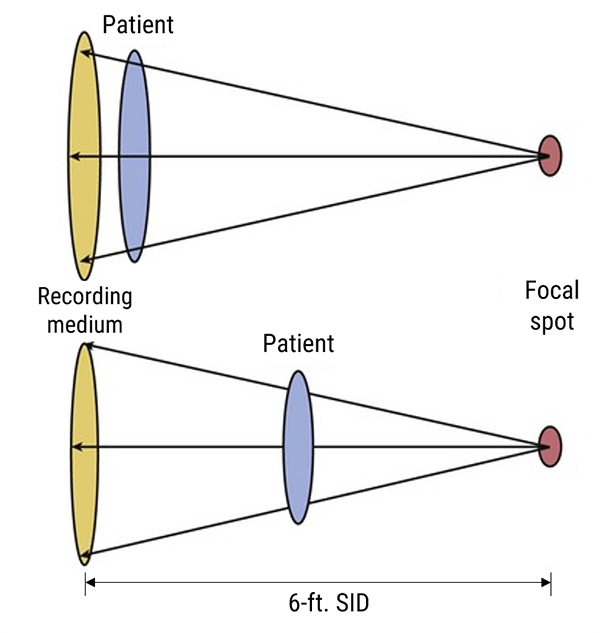
X-rays travel in straight lines in air at a distance of 72 inches from the detector. They diverge in all directions and are attenuated by the housing around the cathode ray tube and by the collimator filters. The structures that the beam hits first, will be magnified in relation to those which are nearer the detector.
Three terms are used to describe positioning: source-object distance SOD, where the object represents the patient; object-image distance OID, where the image is the detector; and source-image distance SID.
To represent an image with as little magnification as possible, the X-ray tube should be placed 72 inches from the image receptor.
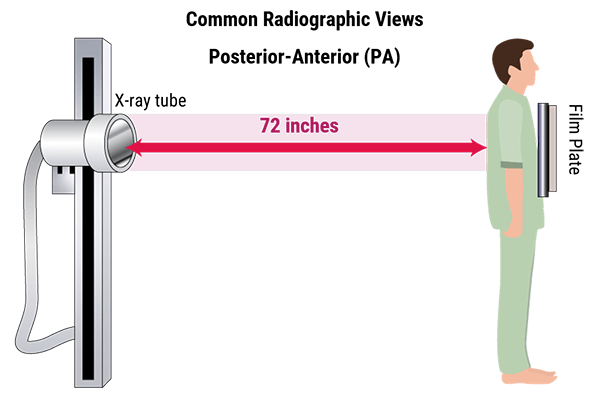
X-ray images are shadows of the anatomy represented on the image receptor. The farther the object is from the image receptor, the more magnified it becomes.
The method of similar triangles is used to show the effects of moving the patient and the detector. To reduce magnification the X-ray source can be moved further away from the patient. Organs that need to be measured accurately, should be placed closer to the detector.
Chest x-ray is one of the most common imaging tests performed in clinical practice, typically for cough, chest pain, and shortness of breath, chest wall trauma, and assessment of occult disease. The two images show the difference between AP and PA images in representing the heart shadow size. Standard x-rays are performed with the patient standing facing the x-ray film or the digital cassette. The tube emits x-rays through the patient from back to front, reducing the magnification of the heart and other anterior structures that are situated close to the film in the PA position.
As a conclusion, a PA beam view of the chest allows more accurate representation of heart size as the heart is positioned closer to the detector and is therefore less magnified.
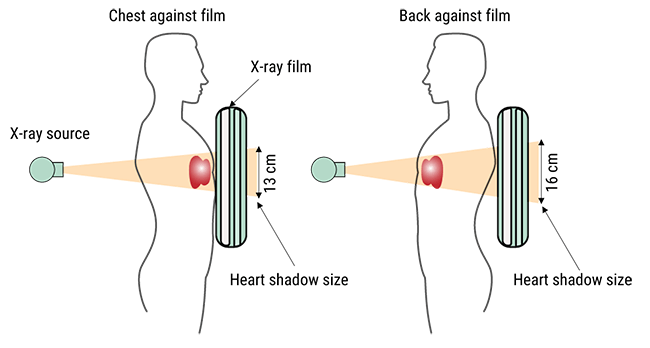
Heart is positioned closer to the detector and is therefore less magnified
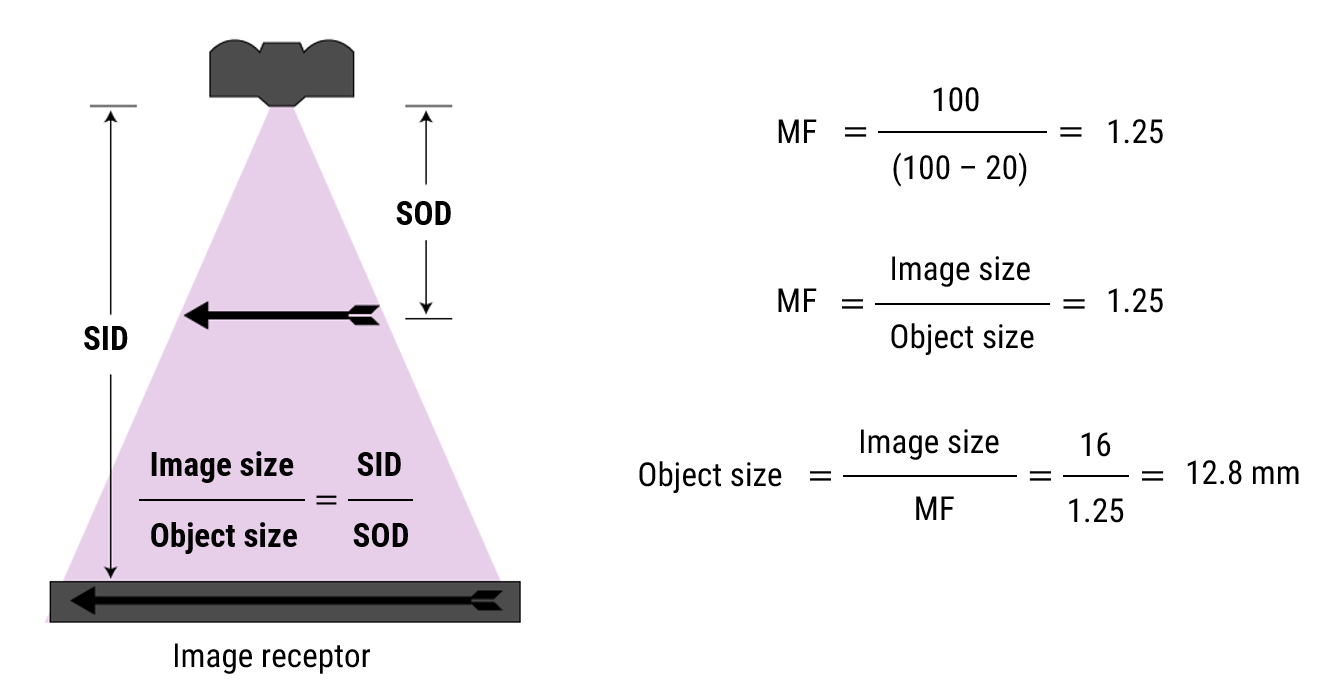
Let’s practice
- SID = 100 cm
- OID = 20 cm
- Image = 16 mm
- Actual size?
Portable examinations shall be performed with the patient’s bed at its lowest height to increase the SID. This will decrease the magnification and represent the patient’s anatomy accurately.
- Positioning of the patient: The SID can’t be controlled to improve the magnification of the organs especially when multiple members of the team are working on the patient simultaneously. It can be difficult to obtain an image with the entire abdomen and pelvis, and pathology may be missed when the minimum SID is not acquired.
- Difficulties of mobile chest X-rays: Ideally, chest studies are performed with the patient in standing position. It prevents blood engorgement of pulmonary vessels, which can compromise image clarity and permits better visualization of air and fluids in the chest. When the patient is imaged while supine, fluids can diffuse themselves across the surfaces of the lung, producing a hazy image.
- The issue of radiation scatter in mobile chest X-rays: The potential degradation of image quality due to radiation scatter occurs when the X-rays penetrate the chest, a percentage of the photons engage in Compton interactions and cause radiation to scatter, resulting in an image with reduced contrast. If a portable X-ray is necessary because of the patient’s clinical condition, then it’s justifiable even if it has potential drawbacks.
There is sometimes a difference between the physician’s orders and what may have been ordered in the computer system. This is why it is important to wisely review the physician’s written order before examining the patient.
While acquiring images, the radiographer has to use his personnel skills to obtain good quality images.
Considerable confusion remains in the radiology community surrounding what constitutes a valid order for a diagnostic test and who must generate that order. The confusion stems from the fact that there are two sets of rules. The Ordering of Diagnostic Tests Rule covers imaging tests performed in a testing facility, and the Conditions of Participation: Radiology Service Rules covers hospital inpatients and outpatients. The physician and the radiographer should respect these two rules for a better communication to avoid misunderstanding which can increase unnecessary exposure to the patient.
As we know, a patient’s exposure to radiation cannot be reversed or undone, so it is important to complete the right examination at the right time.
All questions regarding the examination shall be clarified before beginning, and consultation with the physician is an essential function of a radiologic technologist as it prevents the patient from unnecessary radiation exposure.
Another necessary component in understanding the physician’s orders is ensuring that the images are completed at the right time. If the physician has not indicated a time on the order, then it is usually considered routine and can be done at any time during the day. Orders that need to be performed urgently will be specified by the physician.
You should also remember that certain studies are time specific, meaning that images must be completed on time with a set amount of time between each image.
It is the radiologist who usually determines how much time should lapse between the images, and relies on the radiologic technologist to obtain the images at the correct time. These types of studies are usually scheduled and performed when several radiologic technologists are available.
To clarify, each order shall be accompanied by an appropriate indication for the image, and must be directly related to the part of the body that is being radiated. Nowadays, computerized physician order entry systems are used regularly and have reduced the need for clarification.
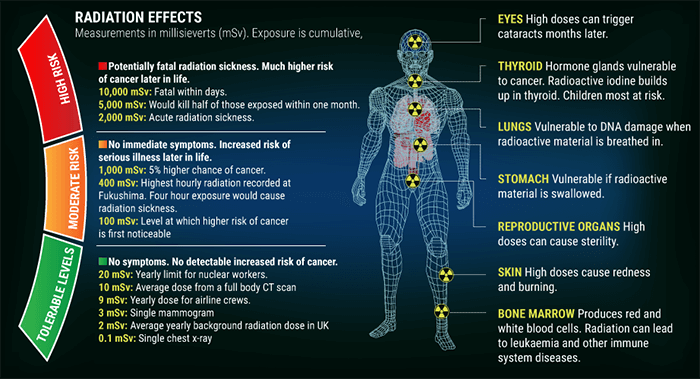
Ionizing radiation damages DNA and has harmful effects on human tissues. Therefore, we will now present the effects of radiation on the patient and provide some practical tips that can help the technologist in reducing the patient dose.
As we mentioned earlier, ionizing radiation damages DNA and has harmful effects on human tissues. These effects can be classified into stochastic and non stochastic effects.
Stochastic effects occur in a linear manner; this risk of injury increases as the dose increases, and the effects are cumulative. They occur by chance with a probability proportional to the dose, and a severity independent of the dose. The most significant risk is cancer.
Non stochastic effects are the same as deterministic effects. They are those for which incidence and severity depends on dose. In fact, after a certain threshold has been met, non stochastic effects occur.
This threshold is the limit at which the organ will be damaged with a polynomial function response.
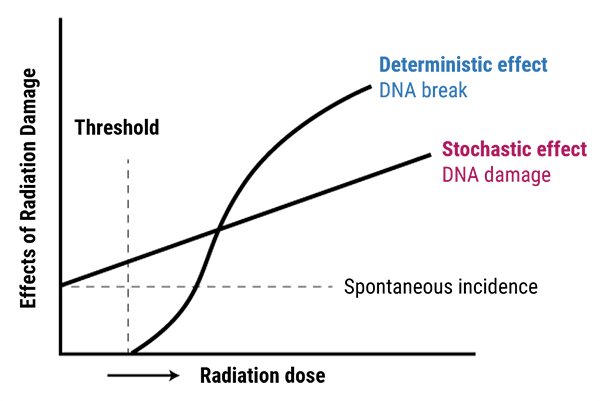
Exposure to very high levels of radiation, such as being close to an atomic blast, can cause acute health effects such as skin burns and acute radiation syndrome (“radiation sickness”). It can also result in long-term health effects such as cancer and cardiovascular disease, if the radiation is in a moderate levels (100-1000 mSv). And finally no symptoms and no detectable risk of cancer are seen if the radiation is in tolerable level (0.1-20 mSv).
The radiation has an effect on the human organs, as we know the organs are divided into two categories the serial organs and the parallel organs. Serial Organs are organs in which disabling any subunit causes the entire organ to fail. In these organs, we have to control the maximal dose to protect all the subunits. (For example, Heart spinal cord)
Parallel Organs, are organs in which many or all of the subunits must be disabled, to cause organ failure .In these organ we have to control the mean dose of the organ, received by a percentage volume of this organ.
- The gastrointestinal tract: Radiation damage to the intestinal tract lining will cause nausea, bloody vomiting and diarrhea. This occurs when the patient exposure is 200 rems or more. The radiation will begin to destroy the cells in the body that divide rapidly. These including blood, GI tract, reproductive and hair cells, and harms their DNA and RNA of surviving cells.
- The reproductive tract: Because reproductive tract cells divide rapidly, these areas of the body can be damaged at rem levels as low as 200. Long-term, some radiation sickness patients will become sterile.
This raises an important question: why do we shield patients?
Patient shielding is an integral part of radiology. Research suggests that improper shielding could lead to repeat exposures, further increasing the patient’s radiation dose. Minimizing radiation exposure to patients is emphasized throughout the radiologic technology profession’s practice standards, and gonadal shielding is considered a best practice.
In fact, a protective shield is placed on the outside of the body to cover the area of the gonads (the testicles or ovaries), and other parts of the reproductive system during radiation therapy. For males, this would also include the prostate and penis. For females, it would also include the fallopian tubes, uterus, cervix, and vagina. Gonadal shielding is a type of fertility preservation.
The radiologic technologist can shield the pelvic inlet as long as the bony structures are not obscured according to the diagnostic needs of the examination. Besides, the shield may obscure the visualization of portions of adjacent structures such as the spine, ureters, bladder, and small and large bowels.
On the other hand for female imaging, the exact location of the ovaries is difficult to estimate, as a result, ovarian shielding is usually impractical.
Radiography maintains to play an essential position in scientific diagnostic. It is important that radiologic technologists understand the proper techniques for acquiring high quality images, regardless of any inherent elements the patient may additionally have.
In addition, radiologic technologists must have a thorough knowledge of abdominal and pelvic anatomy, as well as different body types, and how each body type can affect the position and the size of the organs, which in turn affects positioning and exposure factors.
Moreover, carrying out doctors’ orders correctly is an important component, as it ultimately reduces a patient’s exposure to radiation. Radiation exposure is well known to have harmful effects on human organs; thus, it is important that radiographers use appropriate shielding to protect patients from useless irradiation.
Post-Test & CE Certificate:
Add to CartPrice: $7.00
| ✔ | Approved by the ASRT (American Society of Radiologic Technologists) for 1.75 Category A CE Credits |
| ✔ | License duration: 6 months from purchase date |
| ✔ | Meets the CE requirements of the following states: California, Texas, Florida, Kentucky, Massachusetts, and New Mexico |
| ✔ | Accepted by the Nuclear Medicine Technology Certification Board (NMTCB) |
| ✔ | Meets the ARRT® CE reporting requirements |
As per the ARRT regulations, you have up to 3 attempts to pass the Post-Test with a minimum score of 75%.
Upon the successful completion of the Post-Test (score 75% or more), you will need to fill up a 1 min survey and then you will be able to issue your CE Certificate immediately.
Refund Policy: Non-Refundable


