Infection Control
Objectives:
- Identify the pathologic and the infectious disease processes
- Determine the different modes of transmission of infectious diseases
- Apply the proper methods of prevention against the transmission of infectious diseases
- Identify the most common pathogens at a healthcare facility and their adequate prevention measures
- Understand the process of occupational exposure management
Description:
Radiologic technologists are most often exposed to different infectious patients. For this reason, the National Institutes of Health, and the World Health Organization, set guidelines for the proper use of personal protective equipment and decontamination of reusable medical equipment. In this article, proper hand hygiene including hand washing and hand rubbing techniques, as well as isolation and infection control procedures will be reviewed. Besides, this article shows the role of the radiologic technologist in preventing the transmission of infectious disease processes in healthcare units and highlights the importance of the policies and procedures detailing the occupational exposure management when a technologist got infected accidentally. This article is accredited by the ASRT for 2.5 Category A CE Credits.
The Medical Imaging field has known wide advancements through the last few decades. Thus Medical Imaging became an invaluable tool that helps clinicians in the diagnosis of numerous sicknesses.
Radiologic Technologists frequently encounter patients before diagnosis, which means that they have to be intensely mindful that most patients may have a pathologic or infectious disease. They need to apply standard precautions to each and every patient, as well as follow isolation procedures when they are in place to reduce the transmission risk of diseases.
Standard precautions include performing hand hygiene and wearing personal protective equipment. Appropriate cleaning of the equipment being utilized is fundamental after each patient’s examination, even for patients who are considered sound.
It is critical to always follow infection control safety measures and strict hand hygiene practices when dealing with bodily fluids. Since healthcare units are persistently updating their plans for how to address infectious patients, it is important for Radiologic Technologists to remain updated on isolation protocols, especially that they have a prominent impact in lessening the rate of transmissibility of the infectious diseases.
This course’s purpose is to educate the Radiologic Technologists on the means by which infectious pathogens are spread, and highlight some of the contaminations that can be encountered when working in a healthcare environment.
Microorganisms are common and present everywhere. Those that are capable of causing diseases are called pathogens. Most microorganisms do not cause diseases; many provide some protection against harmful microorganisms.
There are 2 types of microorganisms: Commensals and Pathogens.
Pathogens are harmful and can cause diseases, while Commensals are harmless and provide some protection against pathogens.
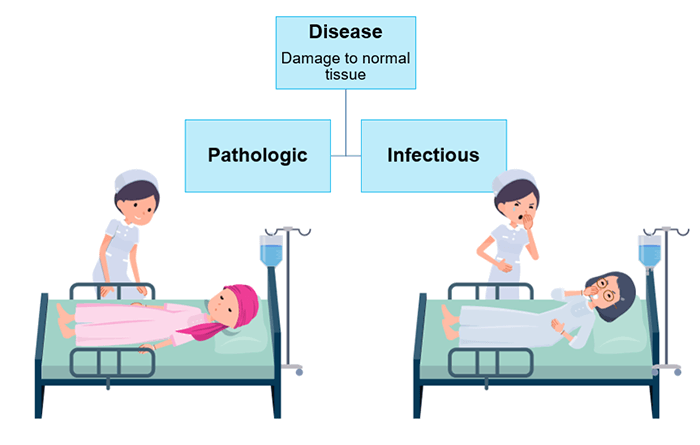
So what is exactly a disease, and what are the types of diseases?
The term disease refers to conditions that weaken or damage normal tissue function. There are 2 types of disease processes: pathologic and infectious. Pathologic processes occur within a single patient and cannot be transmitted from patient to caregiver or patient to patient. Whereas Infectious processes can be transmitted from patient to caregiver or patient to patient.
An example of the difference between pathologic and infectious processes would be a comparison between viral or bacterial pneumonia and Lung cancer. Pneumonia can be transmitted from a patient to a caregiver and is an example of an infectious process. Cancer, on the other hand, cannot be transmitted from a patient to a caregiver and is an example of a pathologic process.
Now that we know the difference between pathologic and infectious diseases, we will explain how does infection occur.
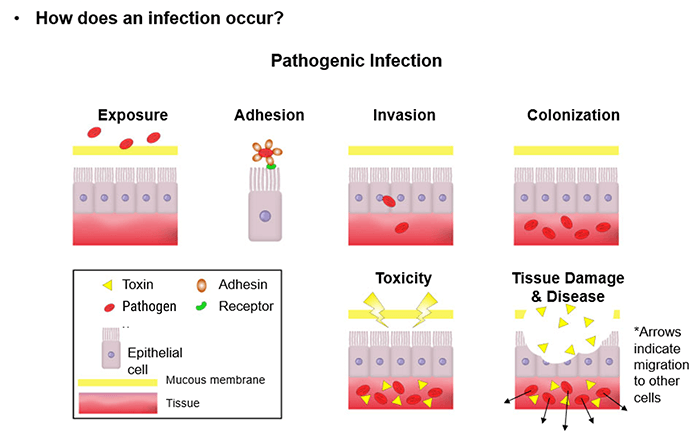
An infection occurs when a pathogen invades and begins growing within a host. To cause disease, pathogens must be able to enter the host body, adhere to specific host cells, invade and colonize host tissue, and inflict damage on those tissues.
This process is composed of 6 steps: Exposure, Adhesion, Invasion, Colonization, Toxicity and Tissue Damage and Disease.
Exposure is the initial phase during which the mucous membrane of the tissue is exposed to the pathogens. The Adhesion phase follows when the Adhesin of the pathogen adheres to the receptor of the epithelial cell. Then, the pathogen invades the epithelial cell and reaches the tissue; this is called the Invasion phase. After the Invasion, the pathogen proliferates inside the tissue; we call this phase the Colonization. The Toxicity phase starts when the pathogens produce toxins that attack the mucous membrane of the tissue. Finally, the Tissue Damage and Disease phase happens when the toxins break through the mucous membrane and the pathogens migrate to other cells.
Understanding how an infection occurs brings a simple question to the mind: how is the body protected from infectious diseases? and when is this protection compromised?
A healthy immune system provides protection against invading pathogens. To function properly, an immune system must detect a wide variety of pathogens and distinguish them from the organism’s own healthy tissue.
People with weakened immune systems are more susceptible to disease; these patients include the very young, elderly, patients with cancer who are receiving chemotherapy, and individuals who have human immunodeficiency virus (HIV) or acquired immunodeficiency syndrome (AIDS).
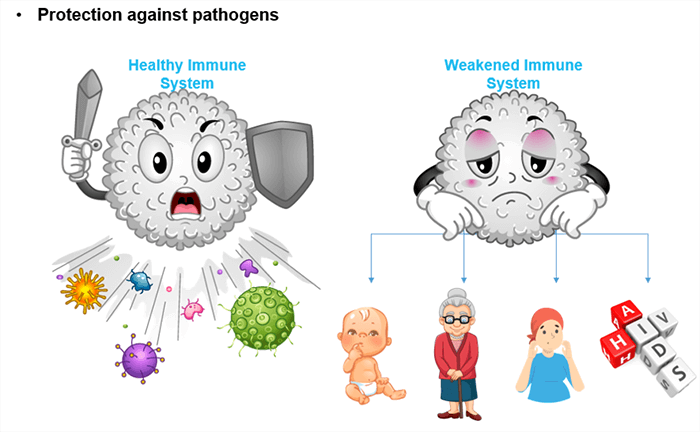
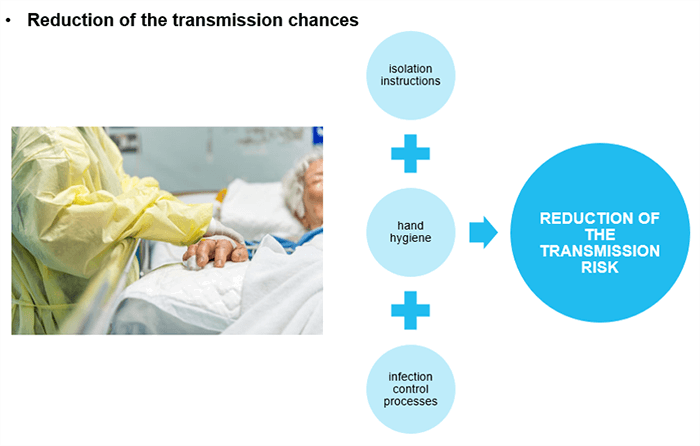
Following isolation instructions, proper hand hygiene, and infection control processes will significantly reduce the healthcare worker’s chances of becoming infected, as well as the chances that these infections will be transmitted from patient to patient.
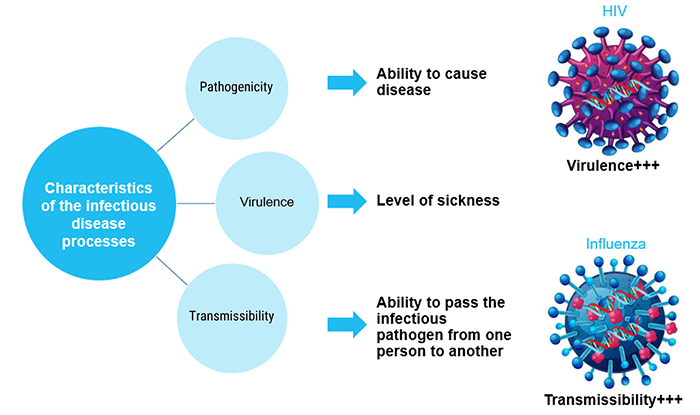
In order to establish effective prevention techniques, it is essential to know the characteristics of the infectious disease processes. The infectious disease processes are characterized by Pathogenicity, Virulence, and Transmissibility.
Pathogenicity is the ability of a microorganism to cause disease in a host organism.
Virulence is the ability of a pathogenic microorganism to cause a serious disease. The level of sickness or disease the infection causes can be very mild and almost undetectable, to very serious and deadly.
Transmissibility is the ability to pass an infectious pathogen from one person to another. Some viruses are easily transmitted, while others are not.
A comparison between HIV and Influenza viruses is a good example to better understand each characteristic: Both viruses are pathogens that can cause diseases; HIV can cause AIDS and the Influenza virus can cause Flu.
AIDS is a potentially life-threatening condition while Flu, in its simple forms, often causes only mild illness. This means that HIV is much more virulent than the Influenza virus. On the other hand, Flu is a contagious respiratory illness that can be easily transmitted between individuals; while AIDS is less transmissible; most of the daily activities pose no risk of HIV transmission. This means that Influenza virus is much more transmissible than HIV.
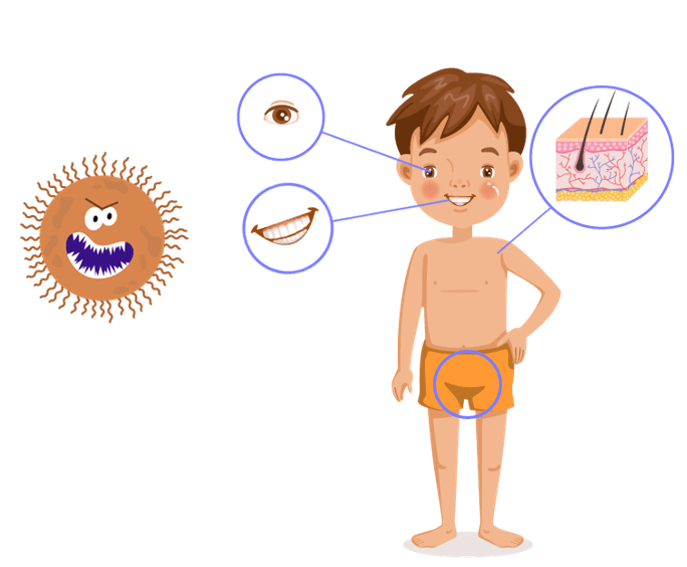
As previously explained, the transmissibility of the infectious disease processes varies depending on the type of the pathogen. Moreover, infectious pathogens follow various modes of transmission between individuals. Viruses typically enter the host via natural orifices, such as the mouth, eyes, or genital openings. Other portals of entry include the skin, through cuts or needle sticks.
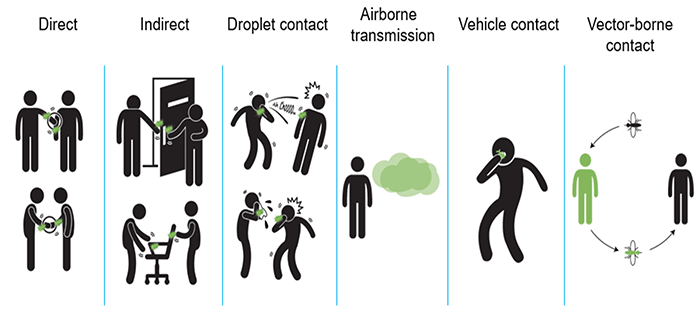
There are 6 modes by which infections are transmitted and corresponding ways of controlling their spread. According to the Centers for Disease Control (CDC) and the World Health Organization (WHO), all infections are spread by means categorized under these modes of transmission. The necessary precautions vary with the microorganism and the context of the illness.
- Direct contact: Transmission by direct contact may occur by touching an infected person and through sexual contact. Direct physical contact is body surface to body surface contact between the infected individual and the susceptible host
- Indirect contact: Indirect contact occurs when a pathogen can withstand the environment outside of a host (the living being that is infected) for a period of time before infecting another individual (a pathogen on an X-ray cassette, countertop, or doorknob). It occurs when an infectious agent is deposited onto an object or surface otherwise known as a fomite and survives long enough to transfer to another person who subsequently touches the item
- Droplet contact: Infectious agents can also be spread through droplet contact via coughing or sneezing and in a healthcare environment during suctioning. Droplets are relatively large and can be projected up to 1 meter
- Airborne without direct contact: Airborne transmission takes place via aerosols that contain organisms in droplet nuclei or dust and can be spread via ventilation systems without direct contact with the host. Examples include tuberculosis (TB), measles, chickenpox, smallpox, and controversially influenza. Airborne transmission takes place through air ventilation without a host present
- Contact with a single contaminated source: Contact with a single contaminated source that spreads the infection is known as vehicle contact. These include point sources such as food or water sources that spread Escherichia coli, or an X-ray image receptor that has the potential to spread bacterial or viral pneumonia, or other viruses and bacteria. Contact with a single contaminated source that spreads the infection is known as vehicle contact
- And transmission by insects or animals: Transmission by insects or animals is called vector-borne contact
Preliminary Actions
The most common modes of transmission in a healthcare unit are from staff to patients, from equipment to patients, or from patients to patients. Proper hand hygiene is the most important barrier against the transmission of infections. The followings are a few preliminary actions to be considered by the Medical Imaging Technologists, and all the staff working in contact with patients:
- Wearing short-sleeved outfits: cuffs of long-sleeved shirts carry more bacteria
- Having short nails without polish: because of their length, longer nails can harbor more dirt and bacteria than short nails; nail polish when chipped may harbor pathogens in large numbers as well, thus potentially contributing to the spread of infection
- Not wearing jewelry: Hand’s jewelry can touch and contaminate wounds or supplies that must be kept sterile or clean
- And covering scratches and lesions with a bandage: exposed scratches and lesions increase the risk of transmission of infections

Hand Hygiene
Indications
As highlighted before, proper hand hygiene is the most important barrier against the transmission of infections; but before detailing the hand hygiene techniques, an essential question is to be answered: When should hand hygiene be performed?
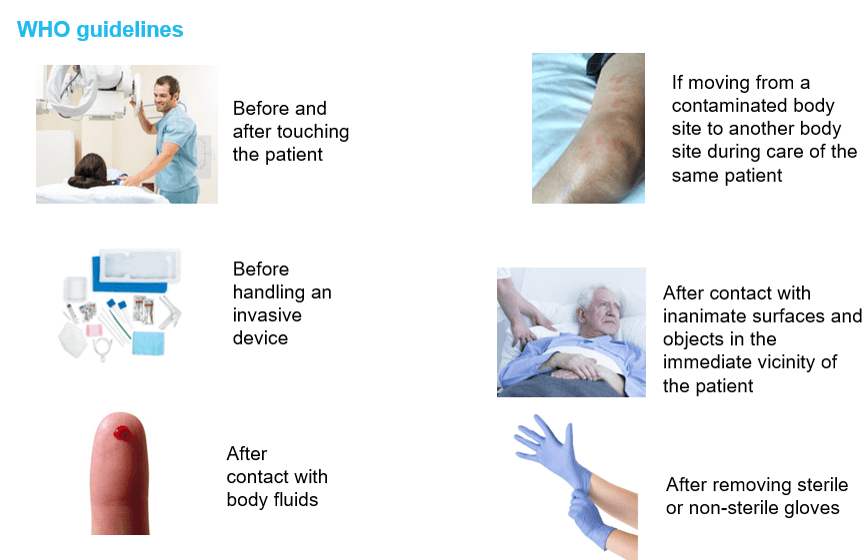
According to the World Health Organization (WHO) guidelines, healthcare personnel, including the Medical Imaging Technologist, should perform hand hygiene rigorously. The following are the indications of hand hygiene that concern the Radiologic technologist in his daily tasks. Hand hygiene is necessary:
- Before and after touching the patient
- Before handling an invasive device for patient care, regardless of whether gloves are used or not
- After contact with body fluids or excretions, mucous membranes, non-intact skin, or wound dressings
- If moving from a contaminated body site to another body site during care of the same patient
- After contact with inanimate surfaces and objects (including medical equipment) in the immediate vicinity of the patient
- And after removing sterile or non-sterile gloves
Hand-Washing
When it comes to hand hygiene practices in a healthcare unit, two techniques are to be discussed: hand washing and hand rubbing. Hands should be washed with soap and water when visibly dirty or soiled with blood or other body fluids or after using the toilet. If exposure to potential spore-forming pathogens is strongly suspected or proven, including outbreaks of Clostridium difficile, hand washing with soap and water is the preferred means. So how to hand-wash?
- First, wet your hands with water
- Apply enough soap to cover all your hand surfaces
- Rub your hand’s palm to palm
- Rub your right palm over your left dorsum with interlaced fingers and vice-versa
- Rub your hand’s palm to palm with your fingers interlaced
- Rub the backs of your fingers to the opposing palms with your fingers interlocked
- Clasp your left thumb in your right palm and rub it rotationally against it. Repeat the same move with your left thumb against your left palm
- Rub your right hand against your left palm rotationally backward and forwards with your right-hand fingers clasped. Repeat the same move with your left hand against your right palm with your left-hand fingers clasped
- Rinse your hands with water
- Dry your hands thoroughly with a single-use towel
- And use the towel to turn off the faucet
- The entire handwashing procedure should last between 40 and 60 seconds, and the duration of the handwash itself should be between 15 and 20 seconds. However, please note that as per the WHO guidelines, you should dry your hands with a clean towel and then use it to turn off the faucet, to avoid contact with bare hands
Hand-Rubbing
Moving to the hand rubbing technique, an alcohol-based hand-rub should be used as the preferred means for routine hand antisepsis if the hands are not visibly soiled. If alcohol-based hand-rub is not obtainable, hands should be washed with soap and water, noting that soap and alcohol-based hand-rub should not be used concomitantly. So how to hand-rub?
- Apply a palmful of the product in a cupped hand, covering all your hand surfaces
- Rub your hand’s palm to palm
- Rub your right palm over your left dorsum with your fingers interlaced. Repeat the same move with your left palm over your right dorsum
- Rub your hand’s palm to palm with your fingers interlaced
- Rub the backs of your fingers to the opposing palms with your fingers interlocked
- Clasp your left thumb in your right palm and rub it rotationally. Repeat the same move with your right thumb clasped in your left palm
- Rub your right hand against your left palm rotationally backwards and forwards with your right-hand fingers clasped. Repeat the same move with your left hand against your right palm with your left-hand fingers clasped
- And once dry, your hands are now safe
The entire hand rubbing procedure should last between 20 to 30 seconds.
Gloves Use
Besides washing and rubbing his hands properly, the radiologic technologist should wear gloves to protect himself from infections. Gloves are a primary line of defense against potentially infectious agents for medical imaging technologists and patients. Patient-to-patient transmission of organisms that cause disease can occur through direct or indirect contact via the hands of the Radiologic technologist or through contaminated patient-care equipment or environmental surfaces.
Gloves protect the Radiologic technologist against infectious agents that could be present on the patients and equally protect the patients against infectious agents that could be present on the Medical Imaging Technologist’s hands. When wearing gloves, it is important to recognize the surfaces that are touched and clean those surfaces with proper disinfectants between patients. Otherwise, if used inappropriately, Gloves present a risk of cross-contamination, and they are not enough to prevent the transmission of infectious disease processes in healthcare settings. Not to forget that hand hygiene must be performed before and after glove use to be effective.

Isolation and Infection Control Procedures
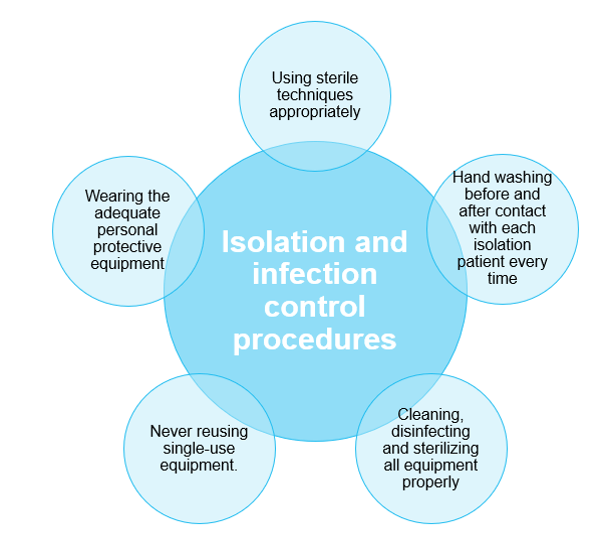
The practices we covered so far if properly performed, help prevent and control the spread of many illnesses; but there is more to the prevention of infection transmission than hand hygiene. Healthcare facilities must have an Infection Control program to help monitor and improve practices, identify risks and proactively establish policies to prevent the spread of infections.
Medical Imaging Technologists, must pay strict attention to isolation and infection control procedures specific to the healthcare facility they work at. This includes the following:
- Using sterile techniques appropriately
- Hand washing before and after contact with each isolation patient every time
- Cleaning, disinfecting and sterilizing all equipment properly
- Never reusing single-use equipment
- And wearing adequate personal protective equipment
Personal Protective Equipment
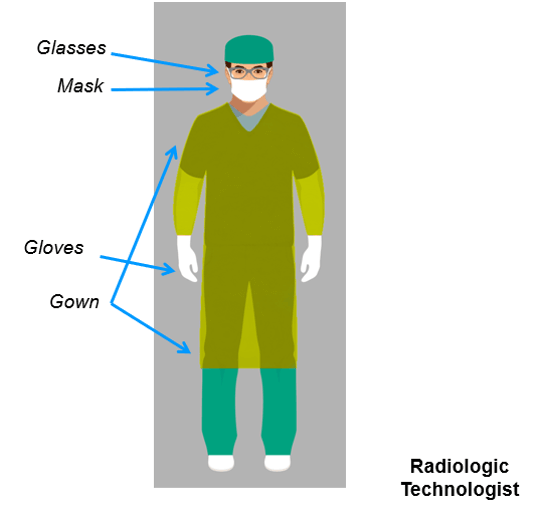
Wearing adequate Personal Protective Equipment (PPE) is necessary according to the isolation and infection control procedures. We will take a look at the PPE that should be worn by the Radiologic technologist when performing his tasks in case of isolation.
Isolation is most commonly used when a patient is known to have a contagious viral or bacterial illness. Special PPE should be used by the Radiologic technologist in the management of patients in the various forms of isolation; the PPE includes glasses, masks, gloves, and gowns.
Cleaning the Equipment
Along with performing good hand hygiene practices and wearing adequate Personal Protective Equipment, Medical Imaging Technologists must clean the used equipment to end the transmission of disease from one patient to another each time an imaging procedure is performed.
Cleaning the equipment is mandatory in between patients, especially the surfaces in the immediate vicinity of the patient. Adequate cleaning material should be used according to the healthcare facility’s infection control policies and special disinfectants must be used in case of isolated patients.
Portable equipment, including portable X-ray and ultrasound machines, image receptors, lead markers, and lead aprons, can be taken to isolation rooms when patients are being isolated for infectious disease processes. At that point, the equipment is moved throughout the hospital, entering both infectious and noninfectious patient rooms. Bacterial and viral pathogens are present on the equipment after being exposed to infectious patients. Without proper cleaning, portable equipment can spread pathogens throughout the healthcare facility. The equipment must be cleaned, adhering to the infection control procedures after imaging is completed. Strict attention must be given to all areas of the imaging equipment regardless of diagnosed or suspected infections to ensure that all surfaces that the technologist and patient came in contact with are disinfected after each and every patient.
An effective way to protect the patient from pathogens that may be on the image receptors is to put these in protective bags. The Radiologic technologist, on the other hand, should be wearing gloves to protect himself. Special attention must be taken to clean the equipment as the patient is often touched with gloved hands and then the equipment is touched with the same gloved hands, thus transferring the pathogen from the patient to the equipment. Even if protective bags are used, the equipment must always be disinfected after every patient encounter.

Most Common Pathogens and Adequate Prevention Actions
Performing proper hand hygiene, using gloves, wearing adequate PPE and cleaning equipment with disinfectants after every patient are important steps to follow, but in many situations, these may not be the only necessary steps. Certain bacterial or viral infections require donning gowns, hazardous material suits, respirators, isolation masks, and cleaning equipment with specific chemicals. It is important to know which bacterial or viral infections require special protective measurements that are above the hospital’s standard precautions.
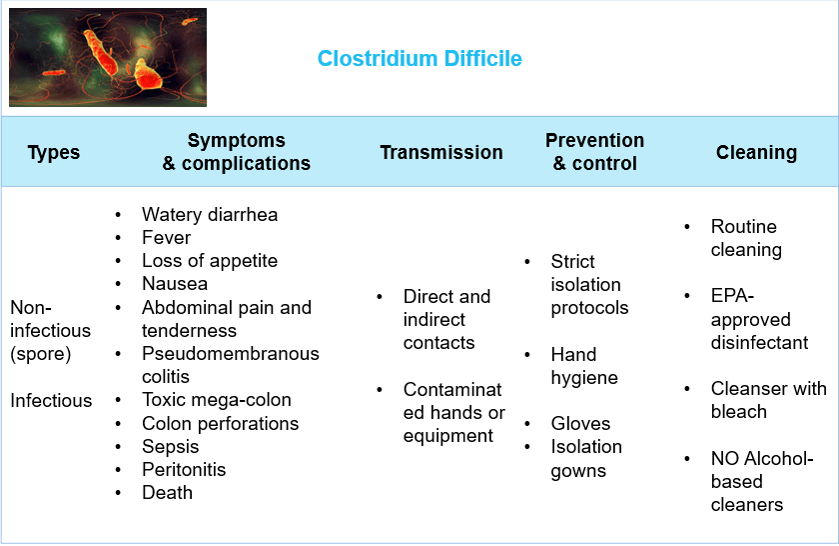
The first common pathogen to cover is a bacterium that causes a serious nosocomial infection: clostridium difficile. A nosocomial infection is a hospital-acquired infection which means that it is contracted during treatment in a hospital or a healthcare unit. Clostridium difficile is one of the pathogens that cause serious nosocomial infections. It is a common bacterium of the human intestine, characterized by a spore-forming, gram-positive anaerobic bacillus. Older adults who have been exposed to antibiotic therapy are at risk for developing Clostridium difficile, as well as patients who have experienced a long-term hospitalization and those with immunocompromised conditions.
There are two existing types of clostridium difficile: a non-infectious form, called a spore, that can survive in the environment for a long time and an infectious form that does not survive for a long time. The spores remain non-infectious until they reach the stomach and the intestines; at that point, they find the correct environment to grow into the infectious form of clostridium difficile.
The symptoms of this infection include watery diarrhea, fever, loss of appetite, nausea, and abdominal pain and tenderness. It can lead to several complications such as pseudomembranous colitis, toxic megacolon, perforations of the colon, sepsis, peritonitis, and death if left untreated.
Clostridium difficile must be ingested and is spread by direct and indirect contact. The spores are primarily transferred to the patients via the hands of healthcare personnel who have touched a contaminated surface. To reduce the transmission of clostridium difficile, Medical Imaging Technologists, and all healthcare workers, are required to adhere to strict isolation precautions, protocols, and procedures defined by their facility when working with infected patients. Hand hygiene, gloves, and isolation gowns should be worn when in the patient’s room and during patient care. Routine equipment cleaning should be performed after every patient, followed by a standard Environmental Protection Agency (EPA) registered disinfectant with a sporicidal claim for environmental surface disinfection. If this is not available, a cleanser with bleach should be used. After cleaning the equipment and removing gloves, hands must be washed with soap and water to remove the spores. An important note to highlight is that alcohol-based cleaners are not effective against Clostridium difficile spores.
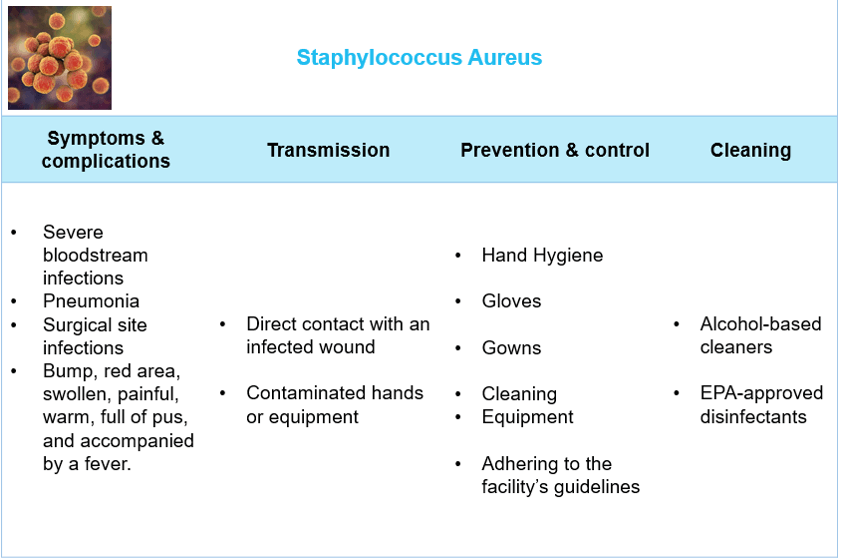
Another very common pathogen that can cause nosocomial infections is the Staphylococcus aureus bacteria. Staphylococcus aureus is a type of staph bacteria that is resistant to antibiotics. It is so called Methicillin-resistant staphylococcus aureus (MRSA) and can cause many complications, such as severe bloodstream infections, pneumonia, and surgical site infections. Most MRSA skin infections appear as a bump or infected area on the skin that could be red, swollen, painful, warm, full of pus, and accompanied by a fever.
MRSA is spread by direct contact with an infected wound or from contaminated hands or equipment. Medical Imaging Technologists and all healthcare workers have the potential to spread the bacteria. In order to break the cycle of transmission, they must clean shared equipment continually and adhere to the guidelines provided by the healthcare facility. Gowns and gloves are necessary when performing patient care, followed by good hand hygiene. Following the protocols and policies set by the facility will protect both the healthcare worker and other patients from the bacteria. EPA-approved disinfectants and alcohol-based cleaners are effective against MRSA and should be used to clean equipment.
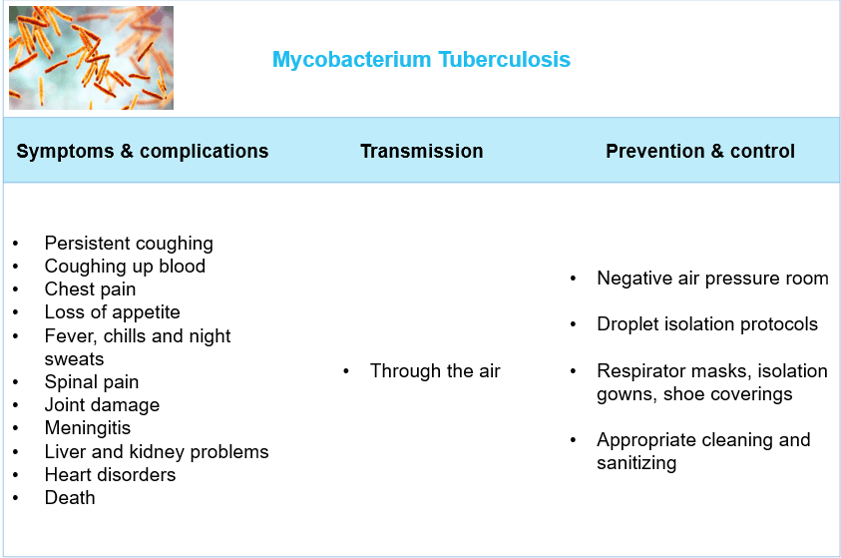
Tuberculosis is a disease caused by a bacterium called Mycobacterium tuberculosis. What are its characteristics and how can its transmission be prevented? Mycobacterium tuberculosis usually attacks the lungs but can attack any part of the body such as the kidneys, spine, and brain. Due to the misuse of drugs to cure tuberculosis, a strain of drug-resistant mycobacterium tuberculosis has become common. Tuberculosis is characterized by a wide range of symptoms: persistent coughing, coughing up blood, chest pain, loss of appetite, fever, chills and night sweats. It can lead to serious complications such as spinal pain, joint damage, meningitis, liver and kidney problems, and heart disorders, and can be fatal if not treated properly.
Tuberculosis is spread between individuals through the air: when a patient who has the infection in the lungs or throat sneezes, coughs or speaks, tuberculosis bacteria are released into the air. At that point, healthcare workers in the same vicinity are able to breathe in bacteria and become infected. To reduce the risk of transmission of tuberculosis, patients suspected or confirmed to have the infection should be placed into a negative air pressure room under droplet isolation protocols. Medical Imaging Technologists, as well as all healthcare workers that are required to enter the patient’s room, must wear isolation gowns, shoe-coverings, and respirator masks that will not allow the transmission of droplets. The appropriate methods of cleaning and sanitizing equipment should be enforced to reduce the transmission of tuberculosis from patients to healthcare workers and between patients.
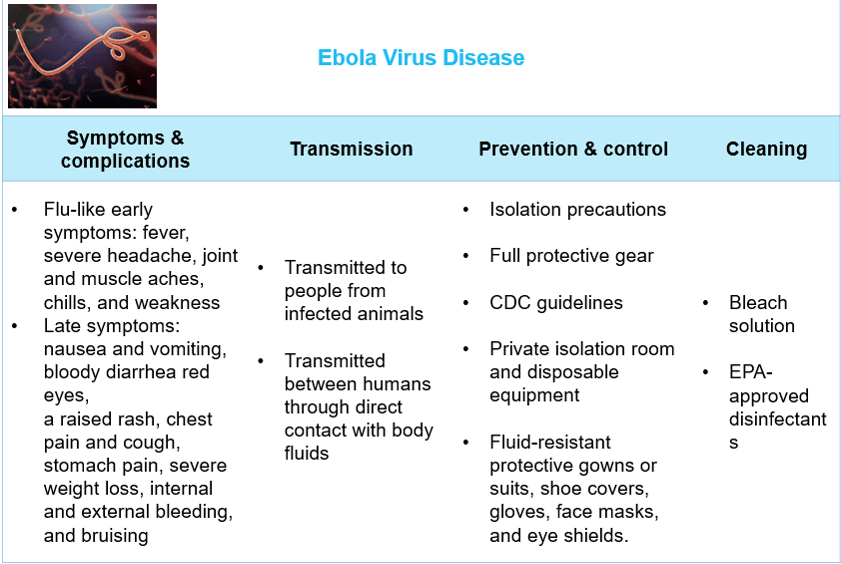
In addition to the bacterial pathogens that we have covered so far, a wide range of viruses can cause serious infectious diseases that require special prevention measurements. Ebola is one of those viruses.
Ebola Virus Disease (EVD), so called Ebola hemorrhagic fever, is an aggressive pathogen that causes a severe, often fatal illness in humans and nonhuman primates. It replicates at an exceptionally high rate which overwhelms the immune system of the host. The World Health Organization states that Filoviridae is the family virus and it includes 3 genera: Cuevavirus, Marburgvirus, and Ebolavirus which has been associated with large outbreaks in Africa.
In the early stages of the infection, EVD presents flu-like symptoms such as fever, severe headache, joint and muscle aches, chills, and weakness. These symptoms progress over time to include nausea and vomiting, diarrhea that may be bloody, red eyes, a raised rash, chest pain and cough, stomach pain, severe weight loss, internal and external bleeding especially from the eyes, and bruising. Early supportive care with rehydration and symptomatic treatment improves the patient’s chance of survival.
The Ebola virus is transmitted to people from the blood, secretions, organs, or other bodily fluids of infected wild animals and spreads in the human population. For example, an animal’s secretions may reside on a piece of fruit that a human ingests, thereby introducing the infection in his body. However, EVD is not easily transmitted between individuals and requires direct contact with blood or body fluids.
Medical Imaging Technologists and all healthcare workers are at risk of being directly infected with the virus while treating infected patients. The Centers for Disease Control and Prevention (CDC) and the World Health Organization are making efforts to put standard care and isolation precautions in place, to lower the chances of healthcare workers acquiring the virus. Special guidelines have been published by the CDC in this context:
- “Prior to working with patients with EVD, all healthcare workers involved in the care of patients with EVD must have received repeated training and have demonstrated competency in performing all EVD-related infection control practices and procedures, and specifically in donning/doffing (removing) proper personal protective equipment (PPE)”
- “While working in PPE, healthcare workers caring for patients with EVD should have no skin exposed”
- “The overall safe care of patients with EVD in a facility must be overseen by an onsite manager at all times, and each step of every PPE donning/doffing procedure must be supervised by a trained observer to ensure proper completion of established PPE protocols”
Strict measures have been recommended when suspected cases of EVD present at any US clinical setting. This includes a private room with private bathroom, single-use disposable equipment or dedicated equipment that does not leave the room, and the use of fluid-resistant protective gowns or suits, shoe covers, gloves, face masks, and eye shields. Using a bleach solution is preferred during environmental cleaning. EPA-approved disinfectants should be used on surfaces that cannot be cleaned with bleach.
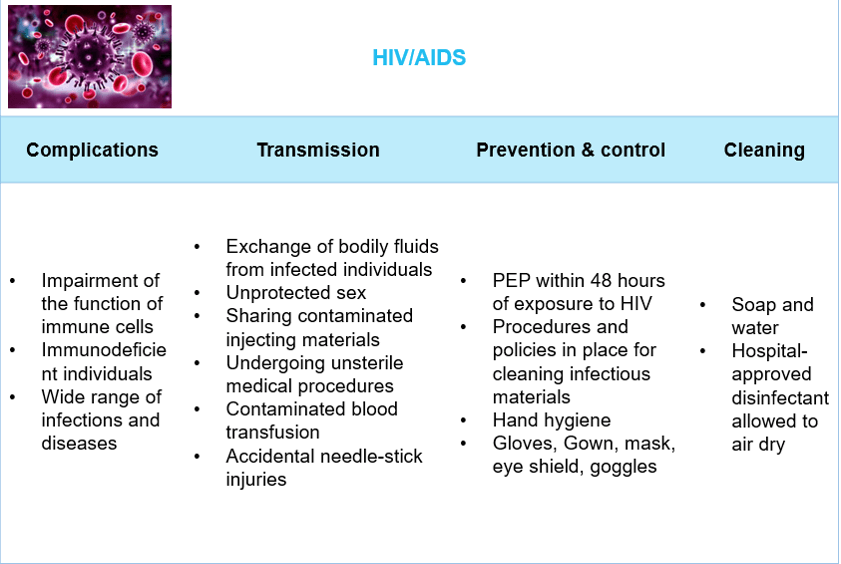
The next viral pathogen to discuss is a major global health issue: The Human Immunodeficiency Virus (HIV).
According to the World Health Organization, approximately 37.9 million people were living with HIV at the end of 2018. HIV causes a chronic, potentially life-threatening condition called acquired immunodeficiency syndrome (AIDS). AIDS can take 2 to 15 years to develop in patients with HIV, depending on the individual. The virus impairs the function of immune cells, which causes the individual to become immunodeficient and susceptible to a wide range of infections and diseases that people with a healthy immune system would normally be able to fight off. Currently, there is no cure for HIV infection, but HIV medicines are available to improve the quality of life of the infected people.
HIV is transmitted through the exchange of bodily fluids from infected individuals, including blood, breast milk, semen, and vaginal secretions. Behaviors and conditions that put people at risk include having unprotected vaginal or anal sex, sharing contaminated needles, syringes, and other injecting materials, undergoing medical procedures that involve unsterile cutting, receiving a contaminated blood transfusion, and accidental needle-stick injuries that are most common among healthcare workers. Ordinary daily contact between individuals such as kissing, hugging, handshaking, or sharing personal objects, does not put them at risk of acquiring the infection. If an HIV-negative person gets exposed to the virus from an HIV-positive person, the prevention of the infection is possible within 48 hours only through the use of antiretroviral drugs; this is called post-exposure prophylaxis (PEP). PEP is often recommended to healthcare workers following needle-stick injuries.
Healthcare facilities have procedures and policies in place for cleaning infectious materials. These procedures should be followed regardless of knowledge of the infectious material; which means that all bodily fluids should be treated as infectious, protective barriers should be used, and waste materials and linens should be properly handled.
Medical Imaging Technologists, as well as every healthcare worker in contact with an infected patient, have to wear adequate Personal Protective Equipment such as gloves, gowns, masks, eye shields, and goggles if splashing and contamination of clothing are suspected.
The area should be cleansed with soap and water, and then disinfected with a hospital-approved disinfectant. To be most effective, disinfectants should be allowed to air dry. Proper hand hygiene should be followed and hands should be washed prior to donning gloves and immediately after removing them.
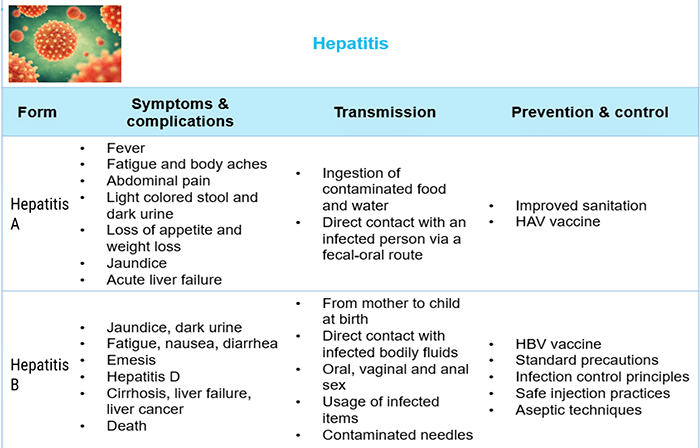
Another common infection caused by viral pathogens is Hepatitis. What is hepatitis? and how could it be prevented?
Hepatitis refers to an inflammatory condition of the liver. There are many possible causes of hepatitis but it’s most commonly caused by a viral infection. There are 5 known types of viral hepatitis: A, B, C, D, and E. Each type is caused by a different virus.
Hepatitis A virus (HAV) is a viral liver disease that can cause mild to severe illness. It is transmitted through the ingestion of food and water that are contaminated by an infected person’s feces, or through direct contact with an infected person via a fecal-oral route. It is one of the most frequent causes of foodborne infection. Sewage contamination is often the reason behind waterborne outbreaks. Generally, the illness isn’t serious and doesn’t cause long-term effects, but it can cause mild symptoms such as fever, fatigue, body aches, abdominal pain, light-colored stool, dark urine, loss of appetite, weight loss and jaundice. In extremely rare conditions, hepatitis A can lead to acute liver failure. Improved sanitation and the HAV vaccine are the most effective ways to battle the disease.
Hepatitis B virus (HBV) is a viral liver disease that causes both acute and chronic diseases. It can be transmitted from mother to child at birth and spreads through contact with infected blood and certain other bodily fluids. Possible methods of transmission include direct contact with infected blood, intimate contact with a person with HBV, oral, vaginal, and anal sex, using any personal item with remnants of infected fluid and being pricked with a contaminated needle.
HBV’s symptoms last several weeks, including jaundice, dark urine, fatigue, nausea, emesis, and diarrhea. The possible complications include hepatitis D infection, cirrhosis, liver failure, liver cancer, and death if not treated properly. The HBV vaccine is the best way to prevent infection.
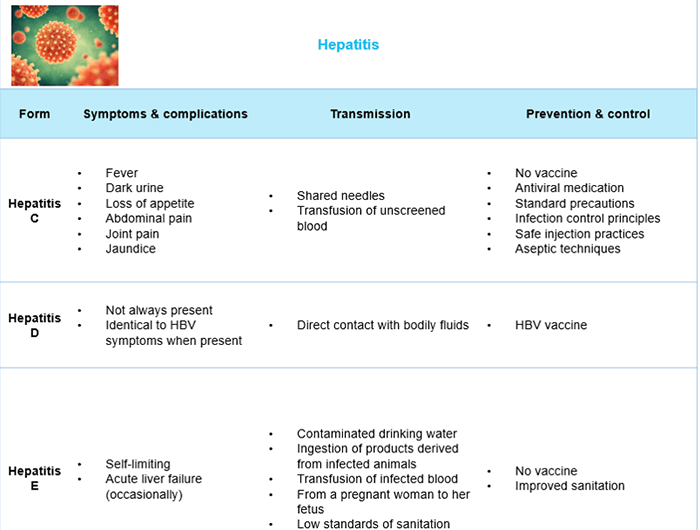
Hepatitis C virus (HCV) is a viral liver disease that can cause acute and chronic infections ranging in severity from a mild illness lasting a few weeks to a serious lifelong illness. HCV is characterized by a bloodborne transmission; it is commonly transmitted through sharing needles and through the transfusion of unscreened blood. Transmissions through sex, from mother to baby and through casual contact are rare. HCV’s symptoms include fever, dark urine, loss of appetite, abdominal pain, joint pain, and jaundice. There is no vaccine for HCV but an antiviral medication can cure it depending on how soon treatment is rendered after diagnosis.
Hepatitis D virus (HDV) is a serious liver disease. It is a very rare form that only occurs in conjunction with hepatitis B infection. It spreads through direct contact with blood and bodily fluids of an infected person such as urine, vaginal fluids, and semen; it can also be transmitted from a mother to her newborn. HDV doesn’t always cause symptoms, but when they occur, they are often identical to HBV symptoms. There is no HDV vaccine, but HBV vaccine is important for prevention because of the conjunction with hepatitis B.
Hepatitis E virus (HEV) is a viral liver disease that resolves on its own within 4 to 6 weeks. Occasionally, acute liver failure develops and can lead to death. HEV is transmitted through contaminated water drinking. More rarely, it can be transmitted by eating products from infected animals and through blood transfusions. An infected pregnant woman can also transfer the virus to her fetus. Low standards of sanitation increase the risk of transmission of HEV.
According to the CDC, “the delivery of health care has the potential to transmit hepatitis B (HBV) and C (HCV) viruses to both health care workers and patients. Outbreaks of HBV and HCV infections have occurred in outpatient settings, hemodialysis units, long-term care facilities, and hospitals, primarily as a result of unsafe injection practices; reuse of needles, fingerstick devices, syringes and other lapses in infection control. To prevent transmission of bloodborne pathogens, health care workers should adhere to recommended standard precautions and fundamental infection-control principles, including safe injection practices and appropriate aseptic techniques”.
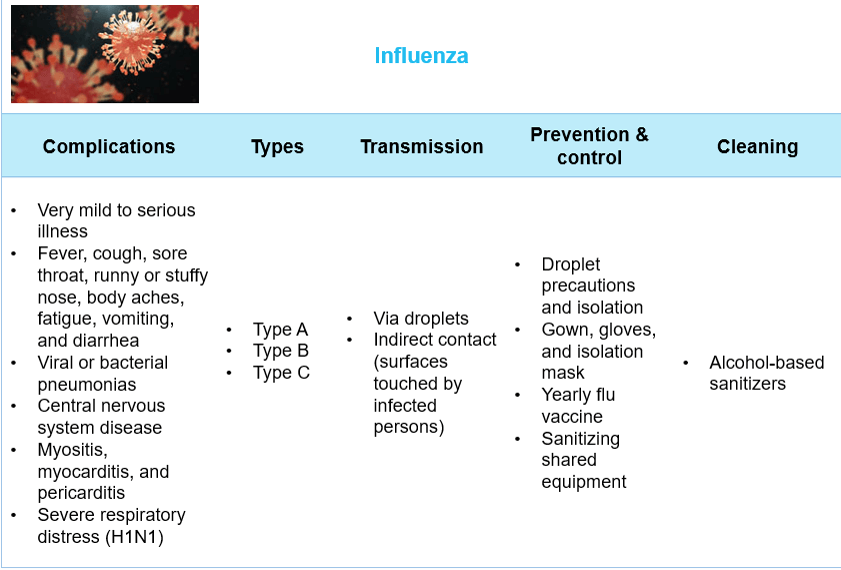
Last but not least, we can’t end our discussion on viral infectious pathogens without bringing up a very well-known and widely spread virus: Influenza.
Influenza, or the flu, is a contagious viral infection that attacks the respiratory system. It takes many forms and variations. There are 3 types of flu viruses: A, B, and C. Type A flu viruses are constantly changing and are generally responsible for the large flu epidemics. They can infect humans and also animals; birds, in particular, are the main reservoir. Type B flu viruses can infect only humans and do not cause pandemics. Type C flu viruses are milder than A and B types and do not cause epidemics. The Swine Flu (H1N1) which had a severe outbreak in 2009 is a subtype of Influenza A.
The flu symptoms include fever, cough, sore throat, runny or stuffy nose, muscle aches, body aches, fatigue, vomiting, and diarrhea. The most common complications of the flu can be viral or bacterial pneumonia, central nervous system disease, myositis, myocarditis, and pericarditis. Adults over the age of 50, children aged 6 months to 4 years, residents in nursing homes, people with compromised immune systems, pregnant women, and people with heart disease are most at risk for flu complications.
Influenza is transmitted via droplets and by touching surfaces or objects that may have been touched by infected people. An infected person may be contagious one day before developing symptoms and up to 7 days afterward. Droplet precautions and isolation are required in healthcare facilities to reduce the transmission risks of influenza.
Different strains of the flu virus mutate over time and replace the older strains of the virus. This is why it’s important to get a flu shot each year to ensure that the body develops immunity to the most recent strains of the virus. The CDC researches and specifies the strains and makeup of the flu vaccine every year. It is highly recommended for Medical Imaging Technologists, as well as all healthcare workers, to get vaccinated. Infection control procedures and protocols should be respected; they are similar regardless of the strain of influenza. Droplet precautions including gowns, gloves, and isolation masks are required, in addition to the disinfection of shared equipment and the usage of alcohol-based sanitizers.
Elements of Post-exposure Management
Despite all the preventive actions that a radiologic technologist can apply to minimize the risk of being infected, coming in contact accidentally with infectious agents whilst carrying out the daily duties is always possible. We will cover the basics of occupational exposure management.
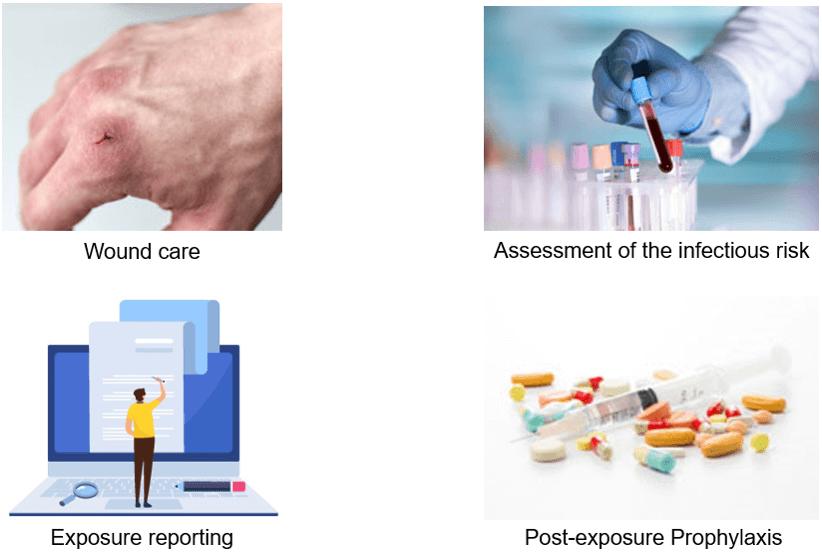
As mentioned previously, each healthcare facility has to set special guidelines and protocols regarding infection control. Among these protocols, there should be clear policies and procedures detailing the occupational exposure management; which means clear steps to follow in case of accidental exposure of a healthcare worker while practicing his duties. These policies and procedures should be posted in visible places and well explained to all the workers during regular training sessions, in order to ensure a correct and quick reaction in case of accidental exposures. The post-exposure management includes four elements:
- Wound care
- Exposure reporting
- Assessment of the infectious risk
- And post-exposure prophylaxis (PEP)
Wound Care
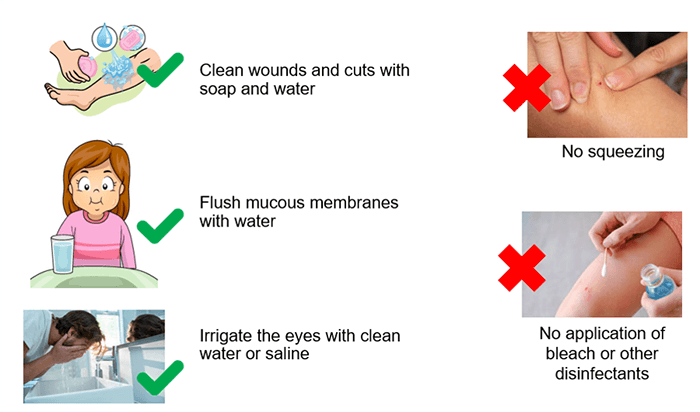
Accidental exposure to infection risks at a healthcare unit can happen in different conditions. A Radiologic technologist can be exposed to accidental needlesticks, sharp instrument cuts and blood or bodily fluids splashing. Any contact with blood or bodily fluids should be considered an exposure to potentially infectious substances.
In case of an accidental needlestick or a cut with a sharp instrument, the affected area should be held down to bleed, and the site or cut should be washed immediately with warm soap and water. The wound should never be squeezed nor soaked with bleach or other disinfectant agents.
In case of blood or bodily fluids splashing, the skin and mucous membranes, such as the nose and mouth, should be flushed with water. If the splashing happens to an open wound or scratch, the area should be washed with soap and water. Clean water or saline should be used to irrigate the eyes if affected by the splashing.
Less frequently, especially when dealing with kids and unstable patients, the Radiologic technologist could be at risk of being bitten; in that case, the wound should be also washed with soap and water.
It is necessary to mention that sexual assault cases require immediate reporting at the Emergency Room department, where they will be held appropriately according to special procedures.
Exposure Reporting
Right after the wound care action that should be done immediately by the affected person, the incident must be reported. What are the necessary details to be included in an exposure report, and to whom shall this report be addressed?
Occupational exposure should be reported as soon as possible to allow for a prompt intervention to reduce the risk of infection. The report should be addressed to the department or individual who is responsible for managing exposures, which is often the occupational health personnel or infection control department.
An exposure report should contain the following information:
- The date and time of the incident
- Details about the procedure that was being practiced at the time of the incident; for example, what was the act of care delivered by the affected person? where was the procedure going on? How did the incident happen? Which device was involved, if any?
- Details about the exposure itself; for example, what is the route of exposure? Which body substance (blood, semen, vaginal fluids…) was involved? What was the approximate volume? How long did the contact persist?
- Information about the source person; for example, name, gender, age, medical ID, hospitalization status (in-patient/out-patient), and previously known medical conditions (medical file)…
Assessment of Infectious Risk
Once the report has been addressed to the responsible person or department, specific steps take place in order to assess the risk of infection related to the reported incident. Let us learn what happens during the assessment of infection risk.
After an occupational exposure, in certain cases, a treatment might be necessary to provide protection against infection. This is why the assessment of the exposed person should happen as soon as possible after the contact incident. Usually, the Infection Control department or the person responsible for managing occupational exposures, initiate the assessment process. Each healthcare facility has its own clear protocol to follow.
The assessment of the infection risk is based on many criteria:
- The type of exposure: percutaneous, mucous membrane, non-intact skin, or bites resulting in blood exposure…
- The body substance: blood, bloody fluid, semen, vaginal secretions, cerebrospinal, pleural, peritoneal, pericardial, or amniotic fluids…
- And the source person’s blood test results: the presence of the surface antigens of the Hepatitis B virus (HBV), the presence of Hepatitis C antibodies, or the presence of HIV antibodies
A very important thing to highlight here is that an informed consent form should be signed by the source person in accordance with state and local laws, in order to do the necessary blood tests. Moreover, any information about the source person should remain confidential.
If the source person is unknown or untestable, the prevalence of HIV and Hepatitis are to be considered in the population group. The exposed person is then sent to the Emergency Room department to be assessed. After signing an informed consent form, his blood is tested for HIV, Hepatitis B, and Hepatitis C. The treatment is then determined based on the criterion mentioned above and the blood test results of the exposed person.
Post-Exposure Prophylaxis (PEP)
Once the infection risk assessment is completed, the adequate Post-exposure Prophylaxis procedure takes place. What is Post-Exposure Prophylaxis? “Post-Exposure Prophylaxis” is attributed to any preventive medical treatment that started after exposure to a pathogen in order to prevent the infection from occurring. This preventive medical treatment can include the administration of medication, as well as vaccines.

PEP for Hepatitis B and C
Now that we know what is post-exposure prophylaxis, we will elaborate its process in case Hepatitis infection is suspected.
To decrease the risk of infection with the Hepatitis B virus, the exposed person may be given a Hepatitis B (HBV) vaccine and immunoglobulin. Hepatitis B immunoglobulin contains antibodies that provide immediate but short-term protection against Hepatitis B virus. The Hepatitis B vaccine provides long-lasting protection by helping the body make its own antibodies against the virus. The exposed person is usually given a single-dose of Hepatitis B immunoglobulin, and 3 doses of HBV vaccine over 6 months. However, if the person has previously been vaccinated for Hepatitis B, and had a blood test documenting response to the vaccine, then no treatment is necessary.
There is no vaccine to prevent infection with Hepatitis C. Blood tests will confirm if the person was exposed to Hepatitis C or have acquired the virus. If the exposed person has a serious cut or wound, the tetanus vaccine may be needed, depending upon the type of the wound and the person’s immunization history.
Follow-up blood tests are required at 3 and 6 weeks, and then at 3 months after the exposure to find out if an infection has been acquired as a result of the incident.
PEP for HIV
In addition to Hepatitis B and C, HIV infection also has a specific post-exposure prophylaxis procedure.
Based on the infection risk assessment, and if the HIV status is unknown, a rapid HIV test should be performed on the patient who is the source of the exposure, after consent has been secured. If the source person is found to be HIV negative, there is no need for further assessment of the exposed healthcare worker. If the result is positive, the healthcare worker needs to be HIV tested. After testing the healthcare worker, if the result shows that he is already HIV positive, then Post-exposure Prophylaxis cannot be helpful. Otherwise, if the result is negative, then Post-exposure Prophylaxis should be administered.
In case of possible exposure to HIV, the health care provider may put the exposed person on a course of antiviral medications without waiting for the blood test results. These medications should be started as soon as possible, and are most effective if started within 2 hours of exposure.
If antiviral medications are prescribed, there is a need for close monitoring to follow, to identify any adverse side-effects of the treatment. The HIV test should be repeated at 6 weeks, 3 months, and 6 months after exposure. If as a consequence of these repeated tests, the healthcare worker is found to have become HIV-positive, then further assessments will be done to administer the adequate HIV treatment and care.

All of the above information leads us to a simple yet very important conclusion: Radiologic Technologists have the ability to reduce the transmission of infectious diseases in their workplace environment. They can fiercely impact the infection control management within their healthcare facility, which means that they can contribute to the creation of healthier hospital settings, that will provide more efficient patient care and improve the quality of treatments.
A simple act of handwashing might not seem a big deal but, if properly practiced, it can save many lives. Together we can make the difference for the sake of our societies. This concludes our Infection Control course.

Post-Test & CE Certificate:
Add to CartPrice: $10.00
| ✔ | Approved by the ASRT (American Society of Radiologic Technologists) for 2.5 Category A CE Credits |
| ✔ | License duration: 6 months from purchase date |
| ✔ | Meets the CE requirements of the following states: California, Texas, Florida, Kentucky, Massachusetts, and New Mexico |
| ✔ | Meets the ARRT® CE reporting requirements |
As per the ARRT regulations, you have up to 3 attempts to pass the Post-Test with a minimum score of 75%.
Upon the successful completion of the Post-Test (score 75% or more), you will need to fill up a 1 min survey and then you will be able to issue your CE Certificate immediately.
Refund Policy: Non-Refundable


