Patient Care and Safety
Objectives:
- Explain the importance of patient care while performing a CT scan
- Discuss contrast media injections and possible side effects
- Describe injection techniques used during CT examinations
- List various types of high-risk patients
- Describe the methods used to measure patient dose
- Understand the role of the CT technologist is reducing patient dose
- Explain why pediatric patients require special consideration
- Discuss the pros and cons of patient shielding
- List methods used in personnel protection
Description:
Patient care is the most important component of any CT examination. This includes communication with the patient, the procedures that are completed prior to starting an exam, during the exam and finally following the CT examination. Since many CT studies include the injection of contrast media, it also covers how to accomplish the venipuncture and injection and the signs and symptoms to look for if there is an allergic reaction of any type during the contrast injection. We will begin by reviewing why communication is so important when doing a CT scan. Also, we will discuss how radiation interacts with matter, the attenuation principle and its relation with the Hounsfield units of various tissues. We will also look at how we measure doses and methods of reducing patient doses in CT scanning. This article is accredited by the ASRT for 1.5 Category A CE Credits.
Patient care is the most important component of any CT examination. This includes communication with the patient, the procedures that are completed prior to starting an exam, during the exam and finally following the CT examination. Since many CT studies include the injection of contrast media, it also covers how to accomplish the venipuncture and injection and the signs and symptoms to look for if there is an allergic reaction of any type during the contrast injection.
We will begin by reviewing why communication is so important when doing a CT scan. Also, we will discuss how radiation interacts with matter, the attenuation principle and its relation with the Hounsfield units of various tissues. We will also look at how we measure doses and methods of reducing doses in CT scanning.
Communication
Communication is one of the most important components of a successful CT examination. We communicate orally, in written format and visually with our patients. The most important step, in the beginning, is to positively identify our patients. It is important to explain the procedure to the patient and follow up with any questions they may ask. When obtaining a patient’s clinical history it is important to note any allergies they may have, especially if they are allergic to latex, iodine, contrast media or seafood.
The history of the patient’s complaints will allow the radiologist to pinpoint areas that may need further study.
We also need to inquire about previously performed diagnostic examinations that were recently completed to make sure that no contrast media was used which may interfere with the CT examination. You must make sure the patient has had NO barium studies in the past 3 or 4 days. Be sure to include a list of the patient’s medications and the last time they took them.
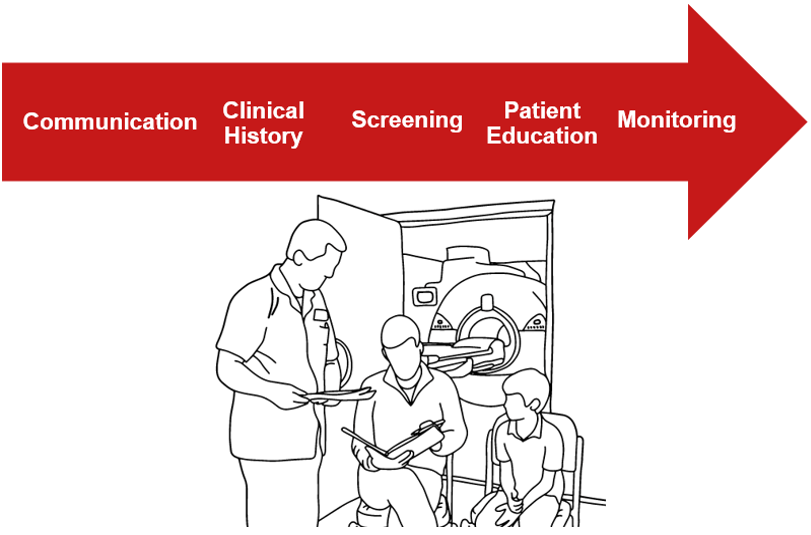
As a technologist, we have many different responsibilities before starting any procedure. Let us review the major steps in preparing for medical procedures, including CT scans, and discuss what we have previously learned prior to doing an invasive procedure.
Pre-Procedures
Role of the Technologist – A Review
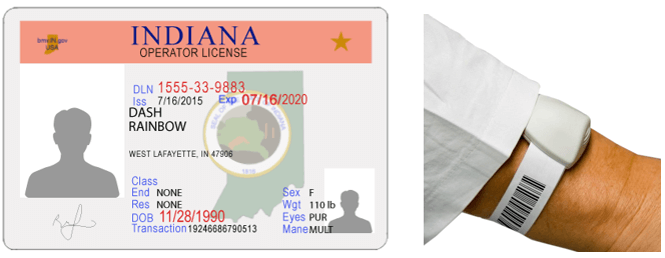
We MUST use at least two identifiers before we ever begin a procedure. Asking the patient’s name, reviewing their wrist ID band, checking their driver’s license if they are an outpatient are some of the ways we can do this. Inquiring about their history of allergies and documenting these is very important especially if contrast media is to be used.
We MUST explain the procedure and answer any questions. Be sure and address any concerns they may have about pain. This will help to ensure the examination goes smoothly. And always remember to monitor your patient during the entire study.
Informed Consent
According to the Code of Medical Ethics Opinion 2.1.1, Informed consent to medical treatment is fundamental in both ethics and law. Patients have the right to receive information and ask questions about recommended treatments so that they can make well-considered decisions about care. Successful communication in the patient-physician relationship fosters trust and supports shared decision making. Medical lawsuits can be avoided in part by always assuring that informed consent in completed and witnessed. Informed consent should be written and signed prior to administering any contrast.

Intra Procedures
During the procedure, it is important to be observant of your patients, especially if they are children. Often people are claustrophobic and this causes stress making it hard for them to lie still.
Claustrophobia
During the procedure it is important to be observant of your patient, especially if they are children. Often people are claustrophobic and this causes stress making it hard for them to lie still. Open CT scanners have been developed and are appropriate for people who are very claustrophobic.

Children present us with additional items to consider when doing a CT examination. While most children 5 or older can hold their breath, practicing prior to doing the exam can help it go more smoothly. Your child may be asked not to eat or drink anything for several hours beforehand, especially if a sedative or anesthesia will be used in the exam. With sedation or anesthesia, your child probably will not be allowed to eat for several hours prior to the exam. In general, children who have recently been ill will not be sedated or anesthetized.
Contraindications
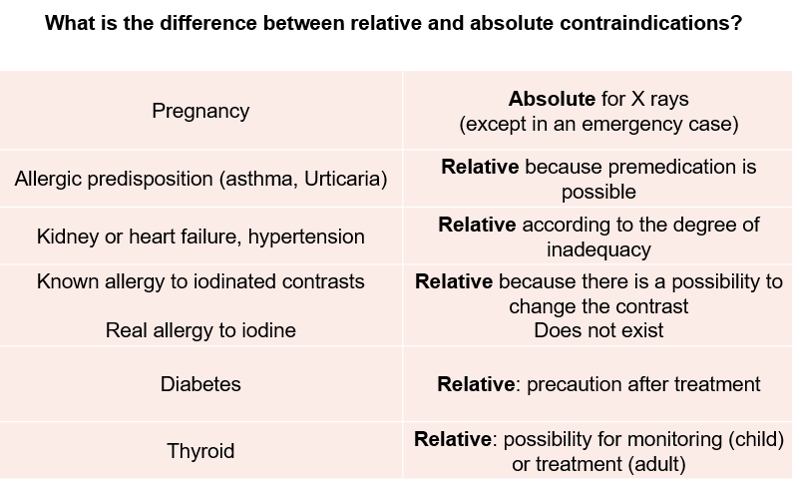
A contraindication is a condition or circumstance that would preclude the use of a CT scan with radiation OR the use of a contrast agent.
Relative or Absolute
An absolute contraindication is a situation that makes a particular treatment or procedure absolutely inadvisable. Relative contraindication means that caution should be used when two drugs or procedures are used together.
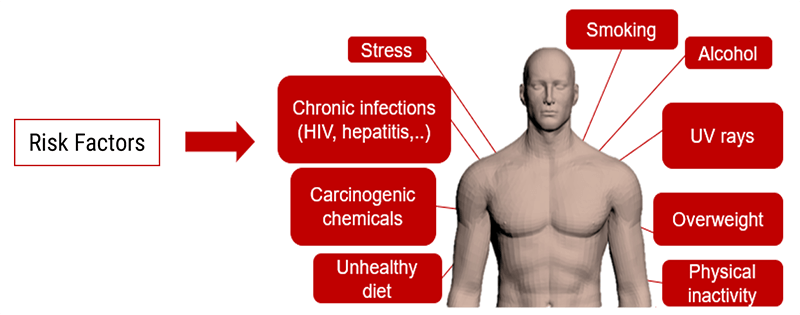
Risk Factors
Identifying patients with risk factors is very important. It is important to identify patients with risk factors in order to take appropriate measures to diminish the importance and consequences of renal failure induced by contrast injection.
For children and elderly patients, the contrast clearance is low. It is important to perform lab analysis prior to any injection of contrast media to verify that renal failure will not be an issue.
High-Risk Concerns
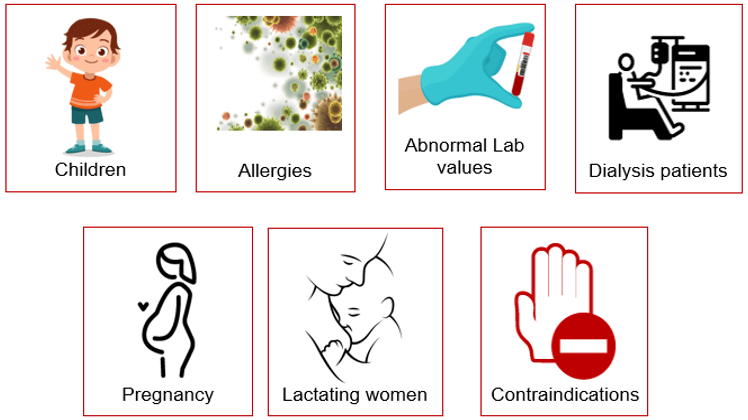
Certain patients are considered high risk and pose additional concerns when using contrast media.
Estimation of Clearance for Adults
When radiographic contrast media are injected intravenously or intra-arterially, they pass from the vascular compartment through capillaries into the extracellular space. They are eliminated almost entirely by glomerular filtration, concentrated in the tubular lumen by water tubular reabsorption, thereby visualizing the urinary tract. But the measurement of creatinine clearance, as derived from 24-hour urine collection, is a cumbersome, impractical, and inaccurate test. The estimated glomerular filtration rate (eGFR) is more accurate and significantly easier to obtain.
- If the clearance reaches 50 ml/min, we can explain to the patient that his kidneys are functioning at 50% of their capacity
- With a clearance of 10 ml/min, replacement therapy has to be considered such as dialysis or a kidney transplant
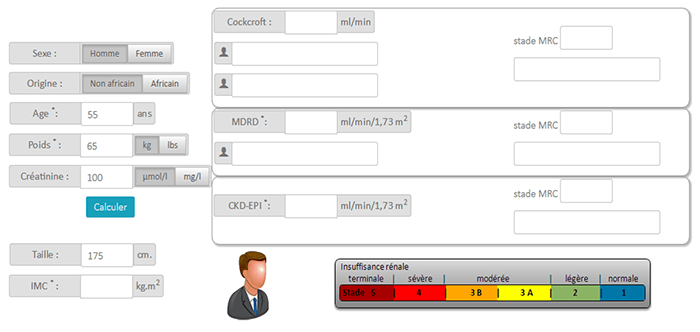
MDRD Formula
MDRD or Modification of Diet in Renal Disease estimates the glomerular filtration rate (GRF) based on creatinine and patient characteristics.
- If male = 186.3 x (creatinemia in (μmol/L) / 88.4)(-1.154) x age-0.203
- If female = 186.3 x (creatinemia in (μmol/L) / 88.4)(-1.154) x age-0.203 x 0.742
- Black race = Result x 1.212
Benefits of the MDRD equation
- A patient’s weight is not necessary. GFR can be calculated from serum creatinine
- GFR estimation is more reliable in the case of older patients
- The international classification of kidney disease is based on the results of the MDRD
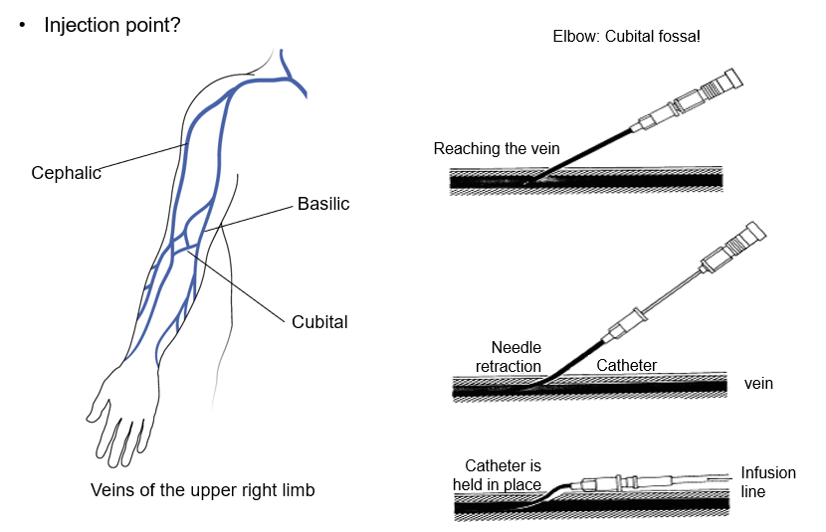
We will talk about venipuncture and injection since many CT studies include the injection of contrast media. It is important to know the signs and symptoms to look for, if there is an allergic reaction of many types, during the contrast injection.
Precaution
If the patient has an IV in place when they arrive to the CT suite, try to inject the contrast media using a different injection site since the injection will be under pressure rather than slow perfusion. This will help to avoid any local complications at the injection site.

Injection
The injection protocol should be optimized for the scan duration. The protocol will determine when contrast enhancement peaks, how long enhancement lasts, and how it varies over time.
- During the acquisition of images, the patient can be injected with a contrast agent (iodine) to artificially enhance the contrast between tissues
- It may be slightly painful and sometimes uncomfortable (sensation of heat immediately after the injection) but usually causes no harm to the patient
Special attention must be paid to patients receiving anti-diabetic treatment.
Tingling in the Arm
Prickling or tingling are the two terms used by patients. The contrast comes “under pressure” in the vein. If the tip of the cathlon is close to the wall of the vein it causes stimulation. This feeling is accentuated for patients who have had chemotherapy as their veins have become more sensitive.
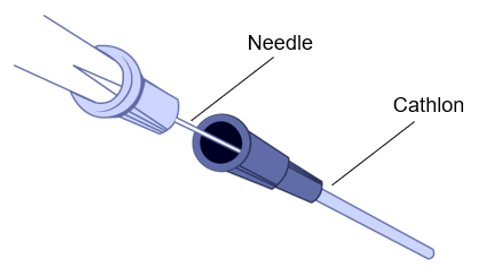
Risk of Extravasation
IV infiltration is one of the most common problems that can occur when fluid infuses into the tissues surrounding the venipuncture site. This sometimes happens when the tip of the catheter slips out of the vein, the catheter passes through the wall of the vein, or the blood vessel wall allows part of the fluid to infuse into the surrounding tissue.
Extravasation occurs when there is accidental infiltration of a vesicant that can cause blistering or chemotherapeutic drugs into the surrounding IV site. Vesicants can cause tissue destruction and/or blistering. Irritants can result in pain at the IV site and along the vein and may or may not cause inflammation. Extravasation can result in tissue sloughing, pain, loss of mobility in the extremity and infection.
The extravasation of contrast agents is an unwanted occurrence that can cause irreversible local injuries.
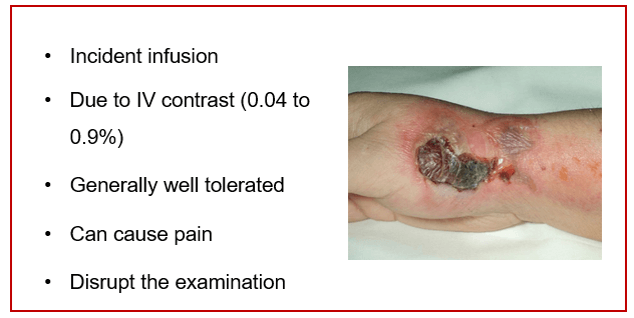
Extravasation of CT scan contrast media into upper extremity subcutaneous tissue is a relatively frequent complication of injection. Contrast extravasation one hour after injection showing a large area in the biceps compartment. Elevation and massage can help with the pain as well as warm compresses.
Contrast Injections
The purpose of contrast-enhanced CT (CECT) is to find pathology by enhancing the contrast between a lesion and the normal surrounding structures.
In the Left image (without contrast injection): organs present similar grayscale preventing proper differentiation of tissues.
The right image shows the contrast agent highlights the different vessels, defines tissues and thus indicates to the radiologist the behavior of the different organs.
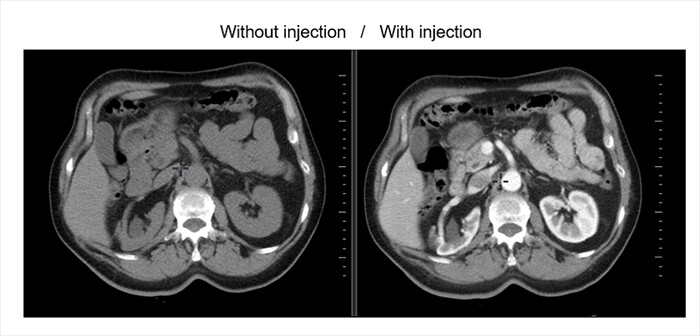
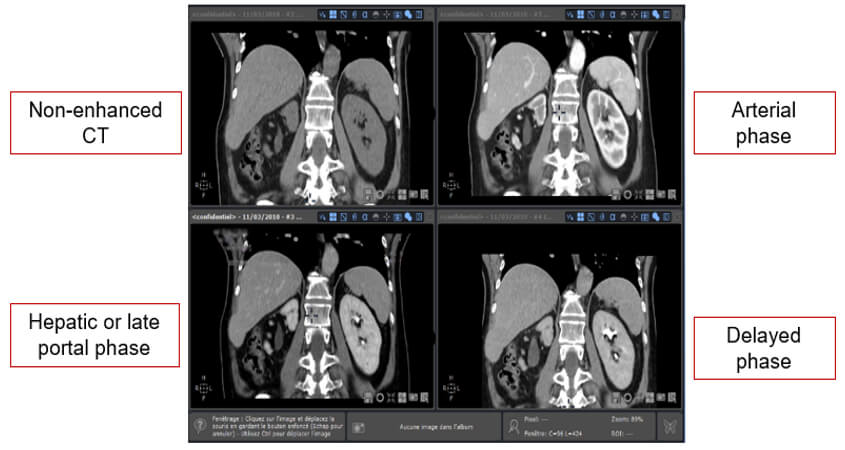
Different Image Phases
Non-enhanced CT helps detect calcifications, fat in tumors, fat-stranding as seen in inflammation like appendicitis, diverticulitis, omental infarction, etc.
The arterial phase is 15-20 sec after bolus tracking. All structures that get their blood supply from the arteries will show optimal enhancement. Hepatic or late portal phase: 50-60 sec after the bolus. Although the hepatic phase is the most accurate term, most people use the term “late portal phase”.
In this phase, the liver parenchyma enhances through the blood supply by the portal vein and you should see already some enhancement of the hepatic veins. The delayed phase is usually 6-10 minutes after the bolus. Sometimes called “washout phase” or “equilibrium phase”. There is wash out of a contrast in all abdominal structures except for fibrotic tissue because fibrotic tissue has a poor late washout and will become relatively dense compared to normal tissue.
Contrast Concerns
Injection
Non-renal acute adverse reactions to iodinated contrast media for CT are flushing, nausea, arm pain, pruritus, vomiting, headache, and urticaria. They are usually mild, of short duration, and generally require no specific treatment. Contrast-induced nephropathy and acute kidney injury are known as renal adverse reactions to CM. These, and anaphylactic reactions, are potentially severe and can lead to death.
Sensation Duration
Patients may feel the first effects of the contrast agent approximately 30 seconds after the beginning of the injection. The peak sensations are usually felt after 50 seconds (in the complete portal phase), then slow down after 1 minute.
Heat Sensation
The venous system is responsible for the heat sensation. This acute adverse reaction, in addition to being uncomfortable, can startle patients who are poorly informed, making it difficult for them to co-operate with breath-hold commands, and decrease the quality of the examination.
- Heat sensation following administration of contrast media is another frequent, but fortunately mild, acute adverse reaction
- Heat sensation produced by high-concentration contrast has been reported to be greater than that produced by medium-concentration contrast
Metallic Taste
When the contrast diffuses into the salivary glands, the patient may taste a metallic taste Please reassure the patient beforehand that this is a normal sensation.
One of the effects of contrast injection may be a metallic taste similar to when we put a silver spoon in the mouth. This is due to the diffusion of the contrast into the salivary glands. This effect is not painful but can surprise the patient.
Vasodilation
The contrast medium will also cause vasodilation, which will cause a flushed feeling. Most patients will notice a very warm feeling that spreads throughout their body for about 20 seconds during and after the injection. This is often concentrated around the groin area and you might think that you are passing urine, but you are not. This is very common, very normal, nothing to worry about and the feeling goes away quickly (10–20 seconds). The reason this makes people feel like they have urinated is because that area of your anatomy has a large blood supply and the warm feeling is slightly amplified there.
Half of the approximately 76 million computed tomographic (CT) imaging examinations performed each year in the US include the use of intravenous contrast agents. There are many categories of patients that we can consider high-risk when discussing contrast media injections. Following an imaging exam with contrast material, the material is absorbed by the body or eliminated through urine or bowel movements. While serious allergic or other reactions to contrast materials are rare, radiology departments should be well equipped to deal with them. Let’s look at those patients in the high-risk category.
Great care must be used when injecting iodinated contrast to certain patients. Contrast-induced nephropathy otherwise known as deteriorated kidney function as a result of iodine-based contrast can have serious effects. Increased morbidity, as well as mortality rates, have been demonstrated in patients at risk. Those patients can include heart patients, diabetics, the elderly and those with known poor renal function and abnormal lab values. Certain precautions should be taken with gravid (pregnant) and lactating women.
Patients with Renal Failure
Clearance is considered to be the amount of liquid filtered out of the blood that gets processed by the kidneys. For kidneys, it is expressed in ml/min.
- The calculation of clearance is important before injection to avoid possible nephropathy induced by iodinated contrast agents
- In the case of CT injection, renal clearance will be the time required to remove the iodinated contrast agent per unit time

Influence of an Iodine Injection on Kidneys
Left Side: Healthy kidney before IV injection – Right Side: Chronic renal failure before IV injection
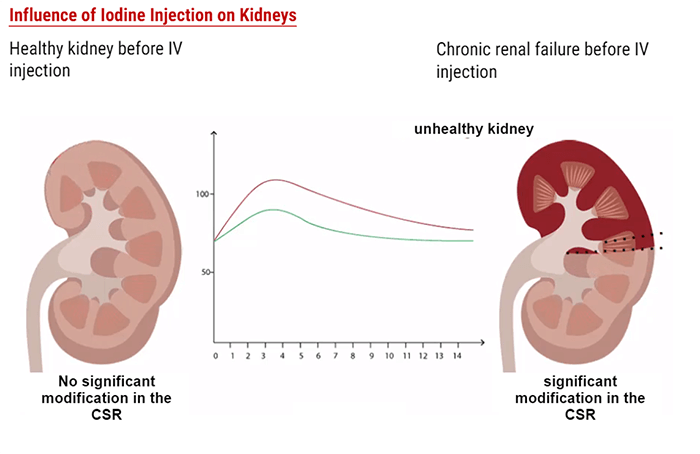
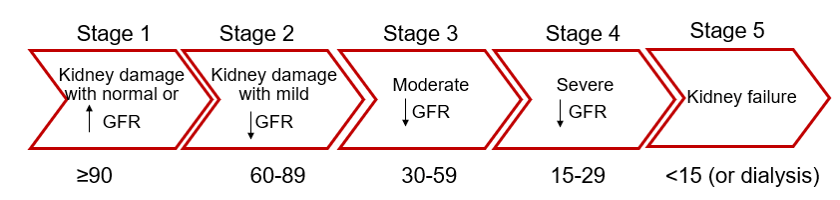
Nephropathy
Depending on the Glomerular Filtration Rate (expressed in ml/min/1,73m2), we can distinguish 5 stages for the kidney function condition. For children and elderly patients, the clearance is low therefore it is very important to perform an analysis on a blood sample before injecting any contrast agent.
Pregnant Women
CT examinations may be contraindicated in patients who are pregnant or suspected of being pregnant unless the procedure benefits out way the risks to the mother and the fetus. When possible an ultrasound should be used. If not possible, or in the case of trauma, a CT scan can be performed with the fewest slices and lowest doses possible to reduce the fetal dose. Always consult a radiologist prior to the examination. Gravid patients pose 2 main problems:
- Radiation exposure to the fetus
- Injection of contrast and its exchange through the fetal-maternal circulation
Breast-Feeding Women
Generally, iodine from iodinated contrast media (either oral or injectable types) is distributed in very small quantities into the breast milk, Approximately 0.04% 1%-2% of the contrast agent ingested by the child is absorbed by his digestive tract. Based on kinetic studies, it is unlikely that these agents will reach therapeutic levels in breast milk, and no adverse effects in infants have been observed following maternal use of iodinated contrast agents.
Both the American Academy of Pediatrics (AAP) and the American College of Radiology (ACR) consider that the use of iodinated contrast media is compatible with breastfeeding.
Lactating women receiving intravascular iodinated contrast may continue with uninterrupted nursing.
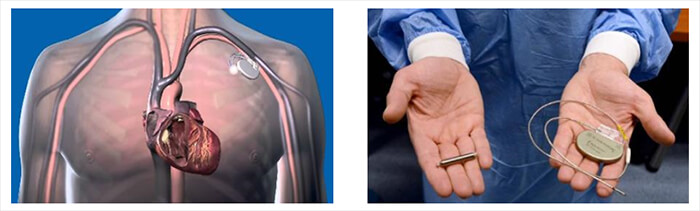
Presence of a Pacemaker
Unlike magnetic resonance imaging, a CT scan can be done even if you have a pacemaker or cardioverter-defibrillator. Although it is possible that CT x-rays directly irradiating the electronics of implantable pacemakers or ICDs can cause electronic interference, the probability that this interference can cause clinically significant adverse events is extremely low.
As contrast media have evolved from ionic, high-osmolality to nonionic, low-osmolality formulations the risk of reactions has decreased over time; however, no pretreatment protocol has been shown to eliminate all repeat reactions. Clinical alertness and early recognition of adverse reactions are of paramount importance and key for the appropriate management of these patients. Adverse reactions occur without warning. They can come in many different forms.
Adverse contrast reactions are typically divided into two categories: immediate reactions and delayed reactions. Immediate reactions, which occur less than 1 hour after contrast administration while delayed reactions occur 1 hour to 7 days after contrast administration.
Allergies
Allergy symptoms may appear within minutes and progress to more serious symptoms, including itching of eyes or face. Varying degrees of swelling of the mouth, throat, and tongue that can make breathing and swallow difficult.
Increasing order of severity:
- Mild: Urticaria, erythema, nausea
- Moderate: Hypotension, tachycardia, dyspnea, vomiting, diarrhea, tachycardia, bradycardia, arrhythmia, bronchospasm
- Severe: Anaphylactic shock
Urticaria
Urticaria is a kind of skin rash recognized as hives. It can be serious if it spreads to the eyes, the mouth, and larynx.
Two basic types of contrast media are used for most radiologic studies: ionic high-osmolality contrast media and nonionic low-osmolality contrast media. The latter has become the preferred form of IV contrast in recent years, given its better safety record, especially for women who are breastfeeding. Urticaria, also known as hives, is an outbreak of swollen, pale red bumps or plaques on the skin that appear suddenly – this is as a result of the body’s reaction to the contrast media used in certain CT examinations.
Reactions to contrast media are not a true allergy, but rather a pseudoallergy in nature, meaning that there is no allergic antibody present that causes the reaction. Rather, contrast media act to directly release histamine and other chemicals from mast cells. The iodine concentration affects the severity of an adverse reaction. The higher the iodine concentration, the greater the risk of an adverse reaction.

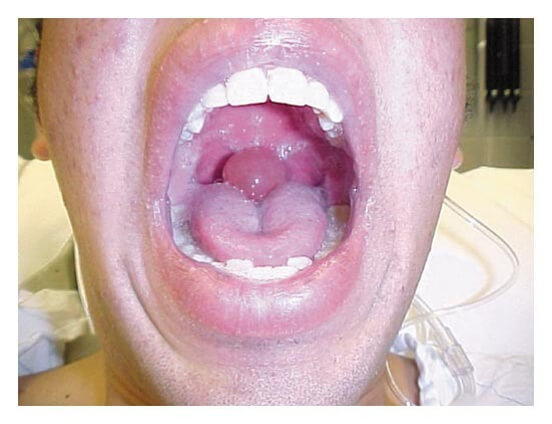
Quincke Edema
Signs and symptoms in patients with Quincke’s angioedema may include the following: Swelling of the face (eyelids, lips), tongue, hands, and feet. Throat tightness, voice changes, and breathing trouble and most concerning a swollen uvula. While rare, this can prevent the patient from breathing and is considered dangerous.
Anaphylactic Shock
Let’s look at the most serious reaction to contrast media to be aware of. The terms “anaphylaxis” and “anaphylactic shock” are often used to mean the same thing. Both refer to a severe allergic reaction. Shock is when your blood pressure drops so low that your cells and organs don’t get enough oxygen. Anaphylactic shock is a shock that’s caused by anaphylaxis.
Anaphylaxis is a serious allergic reaction that is rapid in onset & may cause death. It presents as Involvement of the skin or mucosal tissue plus either respiratory difficulty or a low blood pressure.
Patients exhibit two or more of the following symptoms:
- Coughing: wheezing; hives & tightness in the chest
- Fainting, confusion, weakness
- Fainting, confusion, weakness
- Swollen tongue, throat & trouble swallowing

Why Drink?
The most important prophylactic measure is hydration. Prior to the day of the exam, all patients should be encouraged to have oral hydration which should include water, coffee, and tea.
After the examination, you should drink at least 5 (8-ounce) glasses of water or until your urine looks clear because the contrast agent contains molecules of large sizes. This will help flush the contrast medicine from your body when the test is finished.
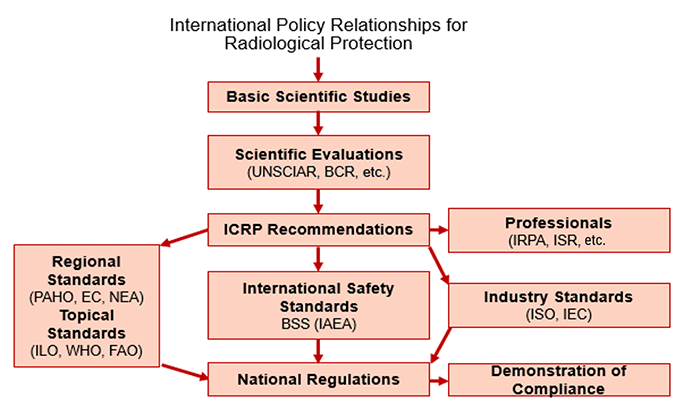
The National Council on Radiation Protection (NCRP) was established to support radiation protection by providing independent scientific analysis, information, and recommendations that represent the consensus of leading scientists.
The International Commission on Radiological Protection (ICRP) is an independent, international, non-governmental organization, whose mission is to provide recommendations and guidance on radiological protection concerning ionizing radiation.
Radiation interaction with matter is the same in CT as it is in diagnostic radiography. The basic units, Rad, Rem, and the Roentgen are terms learned in radiography education but warrant reviewing here. If you recall, the RAD stands for radiation absorbed dose or the amount of radiation that is absorbed by the patient. That term has been replaced by the GRAY which is the Systems International term.
The REM, or roentgen equivalent man, describes the type of radiation a person is exposed to. This term is used in measuring the dosage that personnel working in CT use. That term is now replaced with the Systems International term Sievert.
And finally, the Roentgen which is used to measure how much radiation is in the air. It is important to remember that you will not have to calculate the patient dose as the CT scanners will do this for you. Lets now look at how radiation is attenuated.
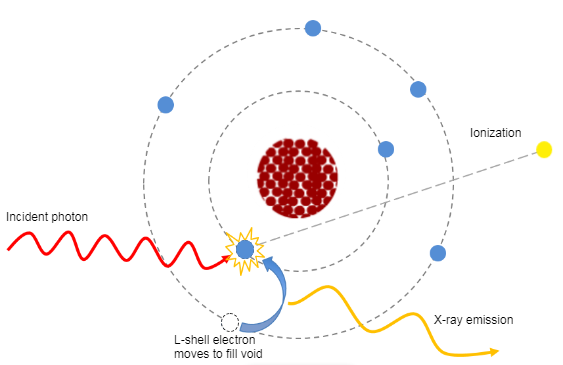
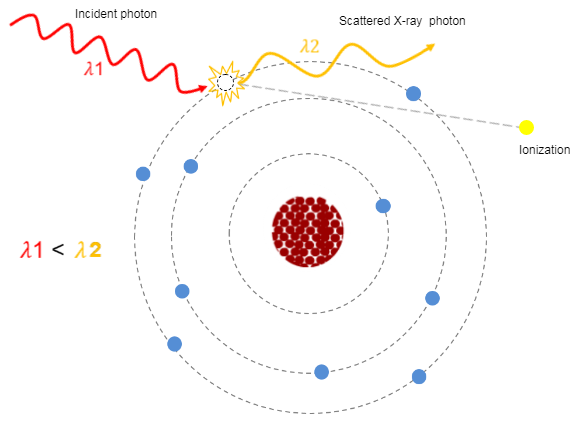
Attenuation is one of the physical principles of radiation interaction. If you recall, it is the reduction in the number of x-ray photons in the beam, and the subsequent loss of energy as the beam passes through the matter (or patient in this instance). In CT, as in diagnostic radiology, the attenuation is dependent on the type of tissue being scanned, such as the soft tissue, the bone, the blood or the muscle. Each type of tissue attenuates a different amount of photons which results in image differences on the finished scan. The denser the tissue, the more the attenuation of the beam.
Let us now look at how the attenuation in a CT scan is measured.
Hounsfield Units of Various Tissues
In 1979 the Nobel Prize was awarded to Godfrey Hounsfield and what was previously known as computed tomography numbers were then named after him. Hounsfield numbers are based on a series of tissue density values calculated by comparing the linear attenuation coefficients of each pixel to that of water. The HU of water is always 0.
This chart demonstrates the average Hounsfield Units of various tissue densities. As we previously stated, the denser the material irradiated, the more the attenuation that occurs in that tissue. By looking at this chart we can see that the denser the tissue, the higher the Hounsfield number assigned, making that area appear more radiopaque or white on the image. The less-dense the tissue irradiated, the smaller the Hounsfield number assigned, causing the area to look more radiolucent or black.
| Tissue | Hounsfield unit |
| Bone | +800 -3000 |
| Kidney | +40 -60 |
| Blood | +15 |
| Water | 0 |
| Fat | -100 |
| Air | -1000 |
Radiation Protection
Many factors affect the dose in CT. Dose reduction, in addition to methods that were developed to account for the variation in patients, has been developed.
How the scan is performed can directly affect the dose deposited into the patient. Patient-specific factors include such factors as age, size, and sex play a role in deposited dosage. We need to discuss the absorbed dose, the delivered dose, and the effective dose.
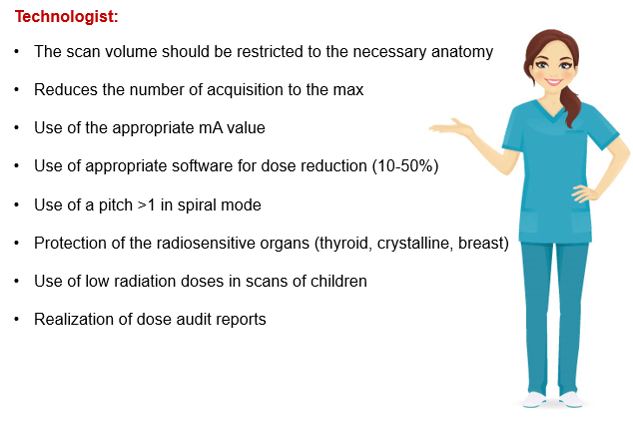
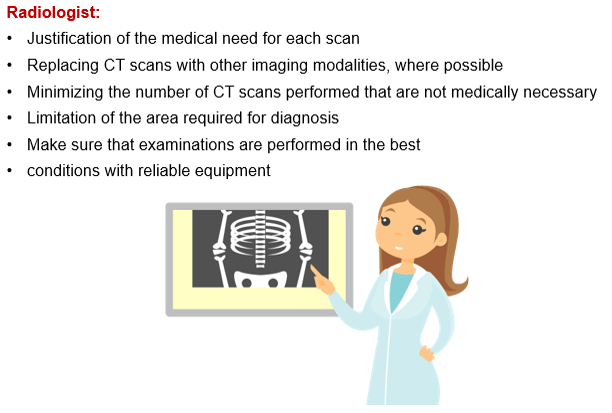
While there are many stakeholders, such as the FDA and the NRC, who oversee patient and personnel safety, the first line of defense in the use of CT dose reduction is the individual facility. Radiologists, technologists, and physicists play an important role in reducing doses during scanning.
Since we have already reviewed the radiation physics involved with scanning, we will now describe how the patient dose is measured in a CT image or procedure and how this dose is affected by the value of the kV, mA, auto mA and pitch. A discussion of the reduction methods used will also help us to understand how to achieve quality images utilizing the lowest doses as possible. Remember, we must always keep ALARA in the back of our minds.
Computed tomography dose index (CTDI)
Computed Tomography Dose Index, known as CTDI, currently is not used but was the original equation used to calculate the patient dose in CT. It was developed by the Federal Drug Administration (FDA)and represents the mean absorbed dose in a scanned object measured in Grays. There is also CTDIv or volume which can be used to calculate dosage from a spiral scan per slice of tissue. Some feel this method may undervalue the dosage given to the patient. The CTDIv is defined by using an acrylic phantom and is not a dose to any actual patient.
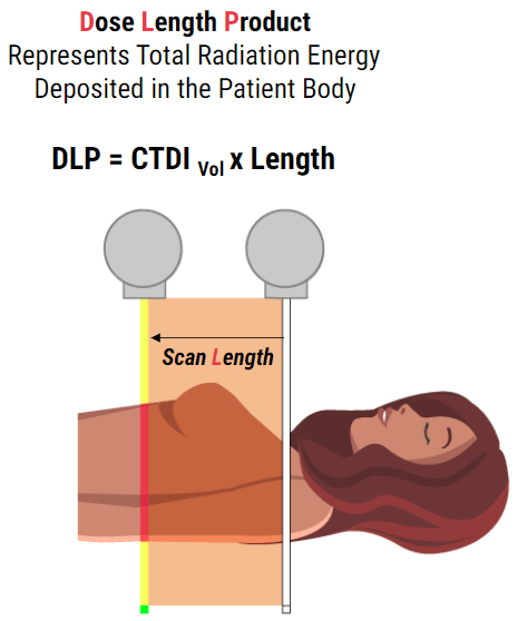
Dose Length Product
Currently, the quantity that is being used as an indicator of patient dose from CT examinations is the dose–length product (DLP). The effective dose can be calculated from the DLP using conversion coefficients that have been proposed for specific routine examinations or by using special software. This gives us the measurement of the total amount of exposure for a series of scans as opposed to one slice. This is dependent on and directly proportional to the scan length. It is the product of the CTDIvol and the scan length.
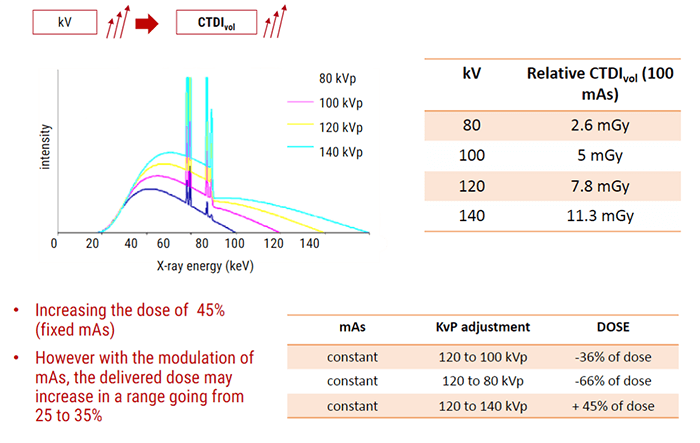
Influence of kV
Subjective Choice of the Technologist
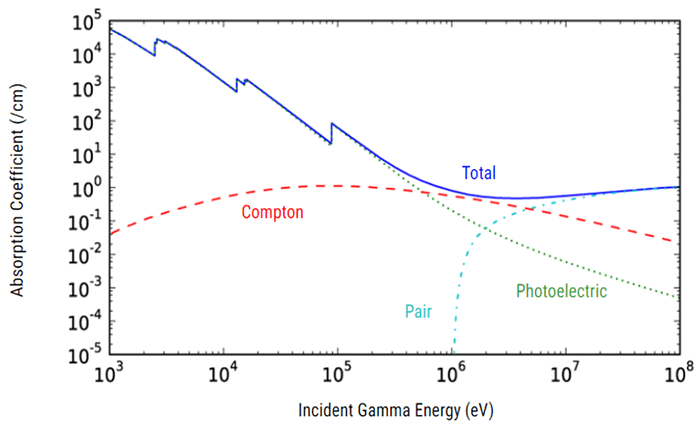
It is important to know that X-ray penetration is an exponentially decreasing function of patient thickness. Thus, large patients will need a much larger dose. We use higher kVp to penetrate large people, large bony people, and bone. As we increase kVp, more of the beam penetrates the tissue with higher energy so they interact more by the Compton effect. This produces more scatter radiation which increases image noise, reduces contrast and increases the dose.
The type of interactions that occur between the patient’s body and the x-ray photons is a function of the selected kVp. Increasing the kVp will improve the signal-to-noise ratio. But decreasing the kVp will reduce the patient dose especially in pediatric and small adults. For contrast resolution of the gray-white matter (or soft tissue) in the brain, the high technique is necessary. Imaging in large patients can be improved also by using the maximum kVp along with an increase in scan time.
Lets now look at mAs and its effect on the dose.
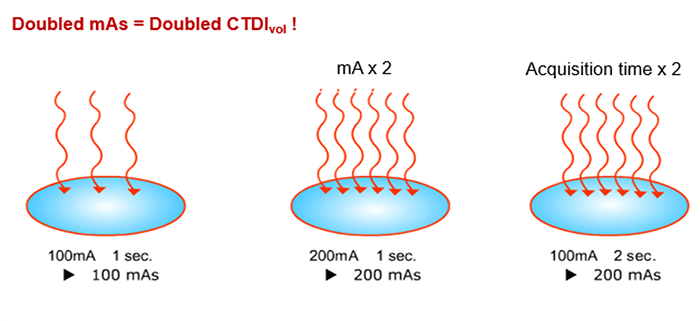
Influence of mAs
CTDIvol is directly proportional to the tube Current and acquisition time. mAs also affects patient dosage. It determines the total number of electrons and only the quantity of the photons is affected by a change in mAs. When mAs is selected, remember that longer scan times will require longer tube cooling and can cause an increase in patient motion. But an increase in scan rotation time will result in better resolution.
The increase of mA and kVp will improve the signal-to-noise ratio but also increase the dose to the patient. Remember, doubling the mAs will increase the CTDIvol.
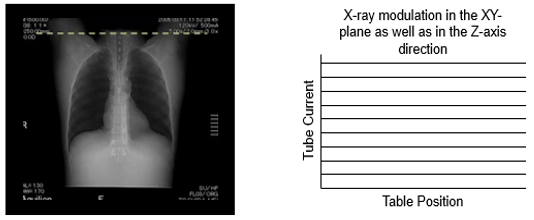
mA Modulation
Automatic correction adjusts dose as a function of patient size and the anterior-posterior and lateral directions. The lateral projection generally encounters more tissue thickness than a PA view. This is known as mA modulation and the mA is increased and decreased as the patient is scanned. Most systems use an average mA to calculate the CTDIvol.
This is an automatic dose-response based on patient anatomy (scout view). Since the human body is not cylindrical, its contours and tissue densities must be taken into account.
Automatic correction adjusts dose as a function of patient size and the anterior-posterior and lateral directions.
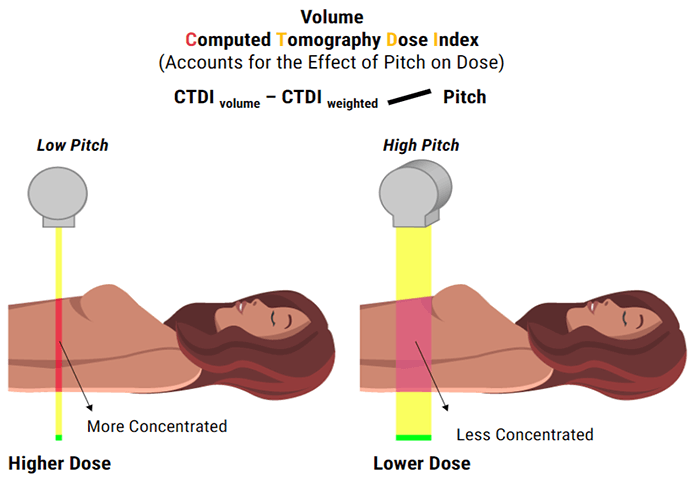
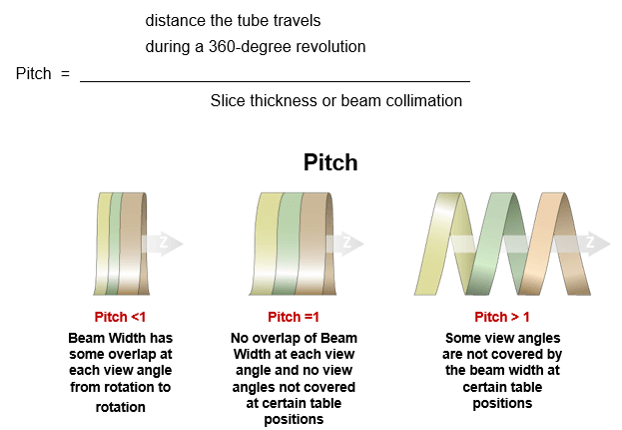
PITCH
Spiral pitch or helical pitch is defined as the ratio of the distance the table travels per rotation to the total collimated x-ray beamwidth. It can also be defined as an extension or contraction of the helix. The pitch has an inverse relationship to the dose. If the Pitch increases by 2, the dose is reduced to one half. It affects not only patient dose but image quality as well.
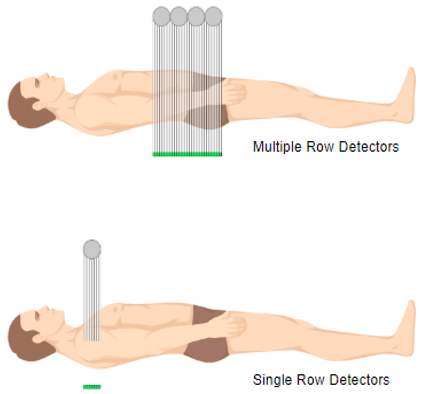
Multi-Detector Configuration
One major problem with a single slice, a single row detector is related to the length of time needed to acquire the data. Multidetector configuration is a form of computed tomography (CT) technology for diagnostic imaging. In MDCT, a two-dimensional array of detector elements replaces the linear array of detector elements used in typical conventional and helical CT scanners. The two-dimensional detector array permits CT scanners to acquire multiple slices or sections simultaneously and greatly increase the speed of CT image acquisition.
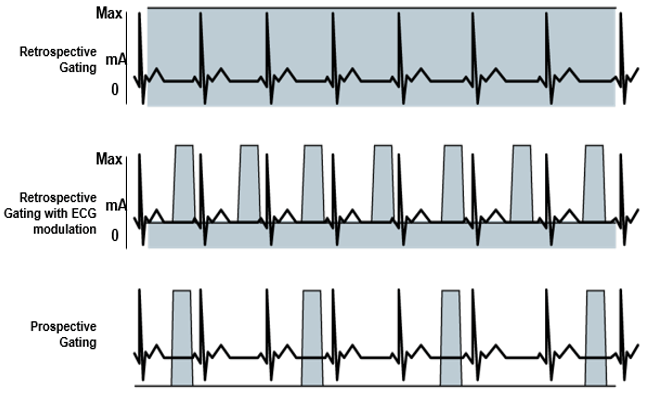
Gating
You should first understand the basics of helical CT. The main challenge in cardiac CT is temporal resolution – in other words, imaging fast enough to ‘freeze’ the motion of the heart. If you are too slow (or image at the wrong time), your images will be blurred by the contraction of the heart.
Gating techniques are used to improve temporal resolution and minimize imaging artifacts caused by cardiac motion. Two approaches to cardiac gating are typically used: prospective ECG triggering and retrospective ECG gating. The least cardiac motion occurs during diastole when the ventricles are passively filling.
In addition to imaging with high temporal resolution, we must image at the correct time – in synchrony with the cardiac cycle. There are two methods of accomplishing this: prospective and retrospective ECG gating. Prospective gating, or prospective ECG triggering, only acquires images during the cardiac diastole; the scanner simply waits in between.
Retrospective gating acquires images continually throughout the cardiac cycle and simply pieces together images from the desired phase (typical diastole for anatomic imaging) after the entire scan is completed. There are advantages and disadvantages to each.
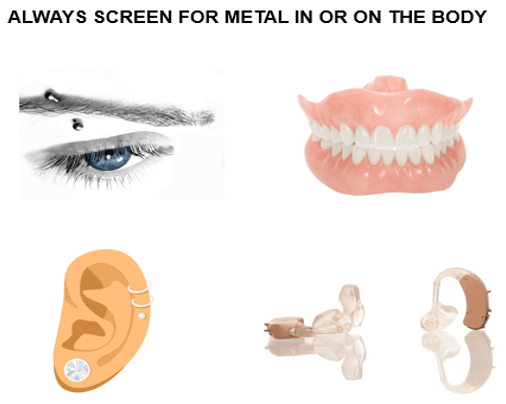
Patient Education
Patient education helps to ensure a quality examination. It is important to inform the patient to lie still during the scan and make them aware of the breathing requirements ahead of scanning. Remember to always screen for the metal in the body to prevent image artifacts. Metal includes hearing aids, body piercings and also dentures that are removable. For their comfort, it is also important to remind them you can see them at all times during the exam.
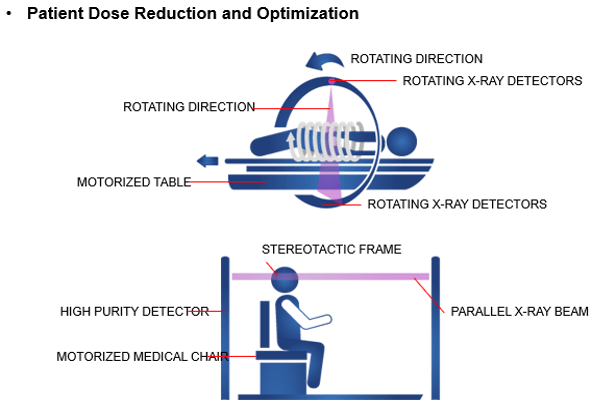
Patient Dose Reduction
The number of CT examinations in the United States has significantly increased in recent decades. The faster gantry rotation cycle times markedly reduced the need for anesthesia in children. In 2008, the Image Gently campaign was founded by the Society for Pediatric Radiology, the American Society of Radiologic Technologists, the American College of Radiology, and the American Association of Physicists in Medicine (AAPM) with the goal of increasing pediatric CT radiation dose awareness by starting a national education and awareness program.
Pediatric dose reduction is important for the safety of children. There are many practices recommended by the Alliance for Radiation Safety in Pediatric Imaging that reduce the dose to children. Such things as scanning only when necessary, reducing the radiation used, asking your medical physicists to monitor your CT techniques and not using multiphase scanning are all important components of pediatric scanning.

Adult Dose Reduction
In 2009, the American College of Radiology (ACR) and the Radiological Society of North America (RSNA) established the Joint Task Force on Adult Radiation Protection to address the safe and effective use of medical imaging and to incorporate dose optimization into all imaging practices Using dose optimization in scanning adults and geriatric patients is the radiation protection principle used to make sure that patient doses are kept as low as reasonably achievable (ALARA). It refers to reducing the radiation dose while keeping the image quality needed to obtain a quality image. Geriatric patients who are very small may need to have pediatric techniques utilized.
- Justification principle – known as the benefit vs. risk principle; an individual’s exposure to radiation should always have a greater benefit and outweigh the negative consequences of the exam
- The benefit of ordering a CT brain for a patient that has suffered significant head trauma outweighs any negative outcomes associated with that exposure
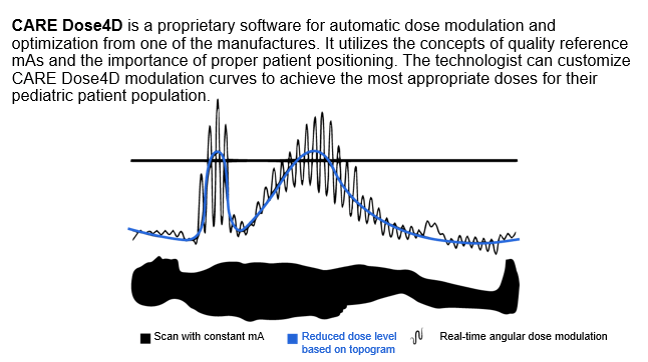
Dose Modulation Techniques
Radiation exposure to the patient has become a concern for the radiologist in the multidetector computed tomography (CT) era. With the introduction of faster multidetector CT scanners, various techniques have been developed to reduce the radiation dose to the patient; one method is automatic exposure control (AEC).
Let’s look at the various dose modulation techniques that are available that help reduces patient dose. CARE Dose 4D (Siemens) assesses the size of the patient cross-section being scanned and adjusts tube current relative to the reference effective milliamperage. It aims to provide adequate image noise, which varies depending on the size of the patient. This system operates on the principle that different-sized patients require different levels of noise to maintain adequate image quality.
SMART mA
Another dose modulation technique is known as SmartmA (GE) which allows the user to set diagnostic image quality by entering the “Noise Index” and a range of acceptable tube current settings (minimum and maximum milliamperage). The AEC system from one vendor, GE, has two elements: AutomA and SmartmA. AutomA provides the patient-size and z-axis AEC elements, and SmartmA provides the rotational AEC element.

SUREExposure
SUREExposure adjusts the tube current appropriately for the selected acquisition and reconstruction parameters and dose reduction algorithms. SUREExposure tube current modulation can reduce patient dose while maintaining image quality.
Radiation Effects
Recent CT scan models have incorporated DoseCheck software which allows the CT technologist to define the notification values (NV) as well as the alert value (AV). This system informs the technologist that the dose exceeds the expected levels before the scan. According to the American Association of Physicists in Medicine (AAPM), Dose notification is defined as the value of the CTDIvol or DLP used to trigger a notification when the value would likely be exceeded by the prescribed scans.
CT Dose Alert is an attribute of CT Dose Check, whereby a value of CTDIvol or DLP can be preset for each CT protocol so that the scanner can alert the operator if the scan settings will yield an estimated dose that exceeds the preset value. This helps to prevent overexposures to the patient.
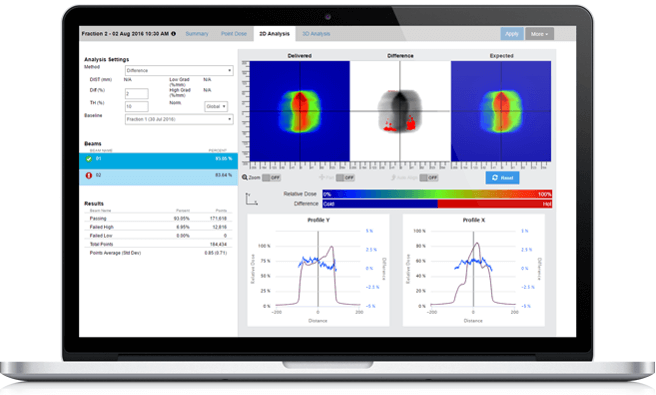
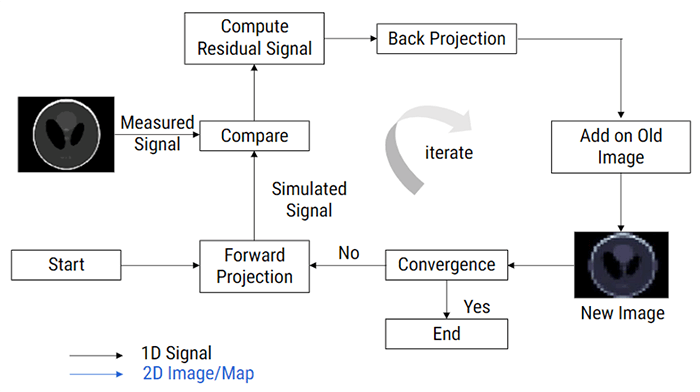
Iterative Reconstruction
Iterative reconstruction refers to iterative algorithms used to reconstruct 2D and 3D images in certain imaging techniques. For example, in computed tomography, an image must be reconstructed from projections of an object. More recently, a much more complex iterative reconstruction algorithm has become available called fully-model-based iterative reconstruction. The implementation of iterative reconstruction can be an important component of overall CT radiation dose reduction – Imaging Wisely – without compromising diagnostic content in CT studies.
Personnel Education
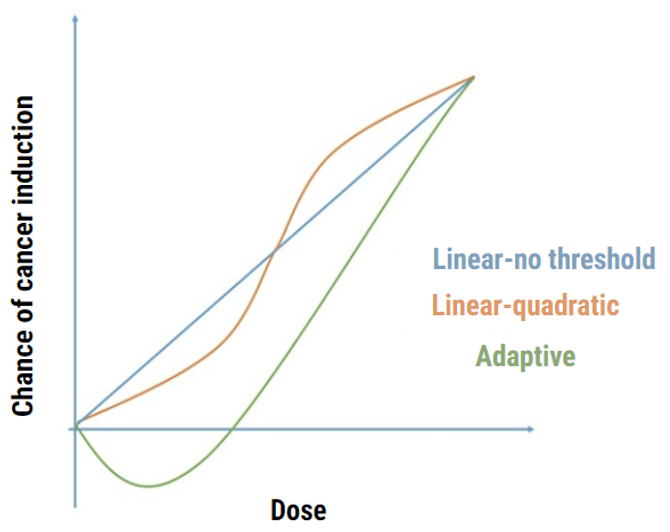
In your previous education, you were taught the bioeffects of radiation. CT technologists must be educated in the radiation bioeffects of the dose in CT. These effects are also classified as deterministic (non-stochastic) and stochastic.
Stochastic effects assume that the probability (not the severity) of the effect occurs depending on the dose. As the dose increases so do the probability and there is NO threshold dose for these effects. If you recall, no threshold means that any amount of radiation can cause some type of effect.
Deterministic effect, such as skin erythema and cataracts, have a threshold dose for which these responses will not occur. Deterministic effects deal with the severity, not the probability of a response.
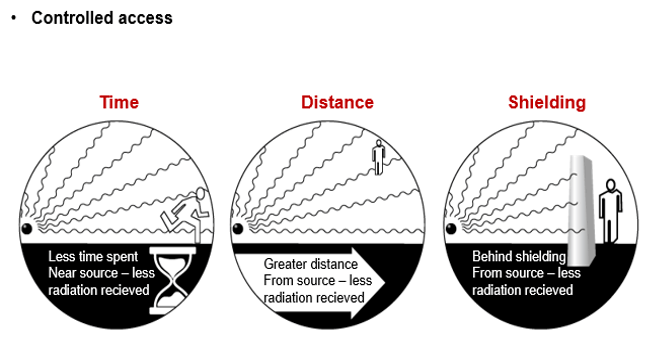
Personnel Protection
Consideration needs to be made to the exposure for operators during CT fluoroscopy. The radiation exposure to personnel can be substantial and equal to patient exposures in fluoroscopy during cardiac catheterization and interventional radiology so protection must be used. The 3 Cardinal Principles of Radiation Protection should be used: Time, Distance and Shielding.
The most significant area of radiation exposure to the radiologist is the hands that will be close to the scan plane during image acquisition while manipulating the needle under real-time imaging. This should be measured using a thermoluminescent dosimeter disc or ring. The absorbed dose to the hands in the direct beam is approximately 1.1 mGy per second. Other organs at risk from a radiation exposure perspective include the thyroid and lens of the eye. Departments will usually have a radiation safety threshold for staff on a per annum basis. Deterministic and stochastic effects could be developed if the radiation exposure exceeds 500 millisieverts per year and 50 mSv per year, respectively.
Shielding
Most traditional shielding, such as lead aprons or pieces of lead, can be used during scanning if no interference will occur in the scan. Lead aprons and thyroid collars are usually used for CT personnel when they must remain in the room during the exposures. It is important to use wrap-around aprons in this instance due to the presence of scatter radiation that comes from the patient.
Thick plated glass in the viewing windows and walls, designed to prevent radiation striking the walls from exiting the room, helps to prevent exposures to CT personnel as well as the public outside the room.

Shielding to protect specific radiosensitive organs in the body lying close to the primary x-ray beam can be used in CT. This includes areas such as breast tissue, thyroid or eye lens. Using Bismuth shielding (non-lead) when appropriate can result in the reduction of the dose deposited into the patient. It is important to remember that this shielding should be used only after the patient has had the CT radiograph (or scout image) completed as this could increase the selection of the automated mA value.

Review of Dose Reduction
Dose Measurement
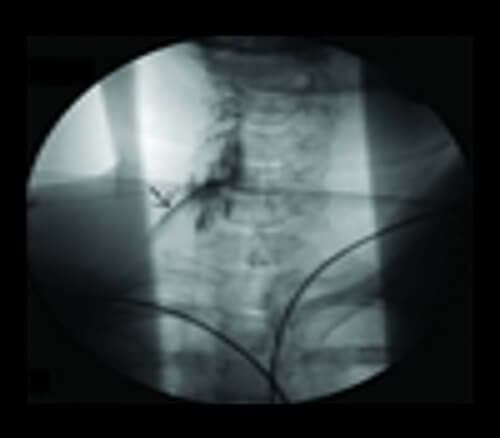
Documentation: Concerns over patient radiation doses are valid. Because CT scans can deposit more radiation dose per examination than other imaging modalities and its use has dramatically increased over the past 10 years, it is important to document doses. Monitoring patient radiation dose must also be performed during Ct guided interventions. In CT-guided procedures, the initial localizing scan contributes the most to effective dose because it is distributed over a large area.
The ability to monitor CT dose metrics is limited by the individual hospital infrastructure and finance, their staff and by the scanner itself. Multiple approaches to gathering data may be required. Estimated radiation dose should be recorded in the medical record, preferably the formal procedure report, for every procedure. Existing Society of Interventional Radiology (SIR) Safety and Health Committee (SIR) guidelines for recording patient radiation dose should be followed.
In reviewing dose reduction methods we now know there are many ways the CT technologist can reduce the dosage to the patient. These all apply to the concept of ALARA and can help in protecting the patients and providing quality examinations. As a CT technologist, you must keep your self abreast of these and all future methods of reducing doses.
Radiologists should justify the medical need for each scan by using the following guidelines:
Post-Test & CE Certificate:
Add to CartPrice: $6.00
| ✔ | Approved by the ASRT (American Society of Radiologic Technologists) for 1.5 Category A CE Credits |
| ✔ | License duration: 6 months from purchase date |
| ✔ | Meets the CE requirements of the following states: California, Texas, Florida, Kentucky, Massachusetts, and New Mexico |
| ✔ | Meets the ARRT® CE reporting requirements |
As per the ARRT regulations, you have up to 3 attempts to pass the Post-Test with a minimum score of 75%.
Upon the successful completion of the Post-Test (score 75% or more), you will need to fill up a 1 min survey and then you will be able to issue your CE Certificate immediately.
Refund Policy: Non-Refundable


