Radiation Dose in Mammography
Objectives:
- Master the anatomy of the breast
- Identify new breast imaging techniques
- Understand how radiation dose is measured in breast screening
- Know how breast density can affect breast cancer diagnosis
- Compare radiation dose levels of each technique
Description:
With the rapid advancement of technology in the medical field and with the application of new breast imaging technologies, including digital breast tomosynthesis, full-field digital mammography, and breast CT, it is important to follow the cancer screening recommendations of the ACR and to understand how radiation dose is measured in breast imaging and which method of measuring and recording dose to the breast is the most effective.
Radiation exposure to the breast may be confusing when considering all these breast imaging techniques. Therefore, radiologic technologists and physicians shall understand the value of a technique before making any decisions about which to use.
In this module, we will show the breast anatomy, discuss different types of breast cancer, show how breast density may affect breast cancer diagnosis, explore different breast screening techniques, explain how radiation exposure can be measured, and discuss radiation dose with each of these breast imaging techniques.
This article is accredited by the ASRT for 1.5 Category A CE Credits.
With the quick advancement of technology in the medical field and with the application of new breast imaging technologies including digital breast tomosynthesis, full-field digital mammography and breast CT, it is important to follow the cancer screening recommendations of the ACR, and to understand how radiation dose is measured in breast imaging and which method of measuring and recording dose to the breast is the most effective one.
Radiation exposure to the breast may be confusing when considering all these breast imaging techniques. Therefore, radiologic technologists and physicians shall understand the value of a technique before taking any decision.
In this article, we will show the breast anatomy, discuss different types of breast cancer, show how breast density may affect breast cancer diagnosis, explore different breast screening techniques, explain how radiation exposure can be measured and discuss radiation dose with each of these breast imaging technique.
We are going to begin this article by discussing the anatomy of the breast.
The breast is well known for being the symbol of femininity with its primary and natural function is to produce milk for breastfeeding.
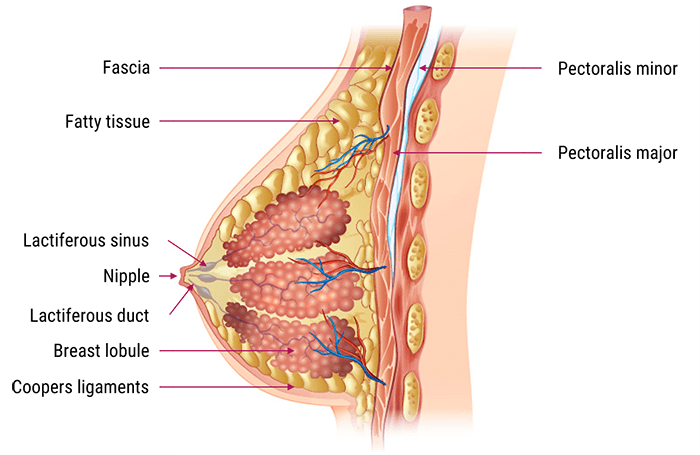
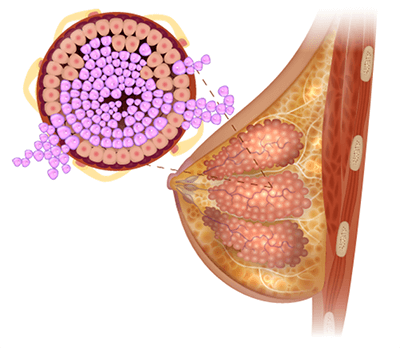
The breast is mostly made of fatty tissues. It is cone shaped having the nipple encircled by the areola at the top of the cone. The base of the cone rests on the chest wall.
The interior of the breast consists of milk ducts, glands, fat, blood vessels and sensory nerves. With the illustration on this slide we can easily locate and identify the shape of the: pectoralis major muscle, breast adipose tissue, lobules with lactiferous canal, nipple, and areola.
The supporting framework of the breast is the coppers ligament which extent from the posterior to the anterior breast.
Let’s go deeper and have a look on the breast tissue.
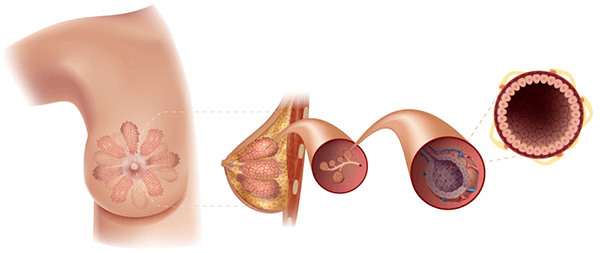
Within the breast tissue are 10 to 15 lobes. The lobes form a tree-like structure of branching ducts that exit at the nipple. At the beginning of the ductal structure is the lobule, in which there are between 10 and 100 acini in each lobule, and that is the secretory unit that secretes the milk during the breast feeding.
The milk produced in the lobules will enter the ducts and travel to the nipple, where the ducts get wider and wider as they approach the nipple.
It is important to note that the acini, which are the milk producing elements of the breast, are only present during pregnancy and lactation.
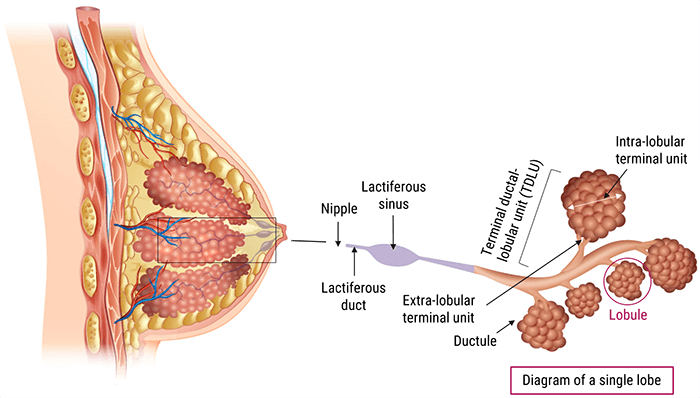
We will zoom in on the lobule which is also called the Terminal Ductal Lobular Unit (TDLU).
- The extra-lobular terminal duct, which is surrounded by elastic tissue lined by columnar cells
- The intra-lobule terminal duct which has cuboidal cells and holds the alveolar glands
The acini is located within the alveolar glands of the lobules, where the acinus is the milk producing element of the breast.
Milk produced in the acini will enter the ductal system and exit at the nipple.
In one sentence: The lobules represent the glandular structure of the breast which are surrounded by adipose (fatty) tissue.
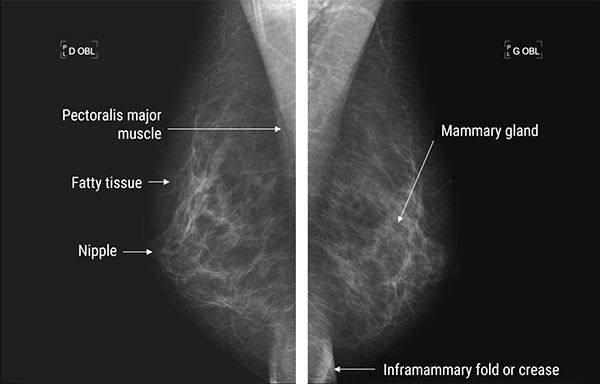
This mediolateral projection of the breast shows the petoralis major muscle, fatty tissue, the nipple and the inframammary fold or crease. Mammary glands are represented by the glandular tissue.
After covering the anatomy of the breast, let’s move now to this new section where we will discuss the different types of breast cancer, then show some statistics.
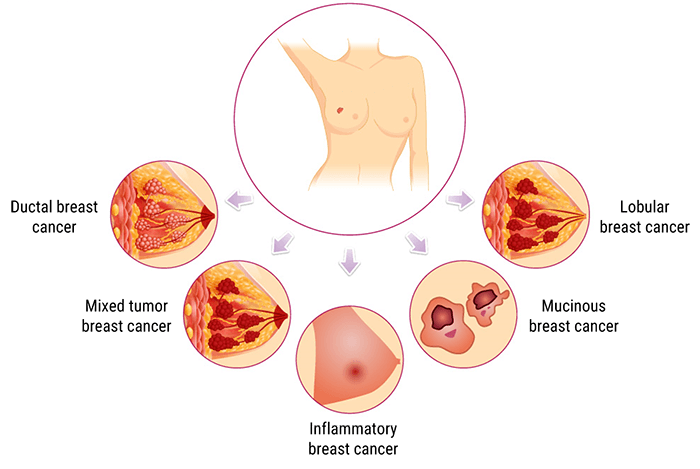
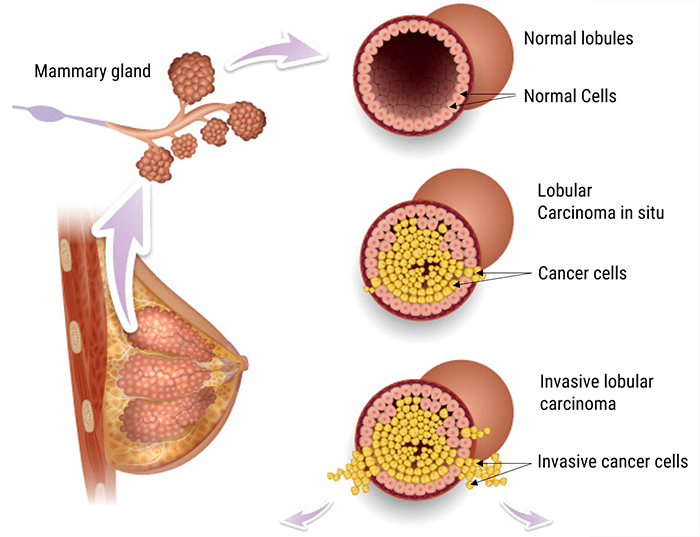
The majority of breast cancers develop in the terminal ductal lobular units (TDLU).
Cancers can also develop in the large ducts, and less commonly in the fibrous or connective tissue.
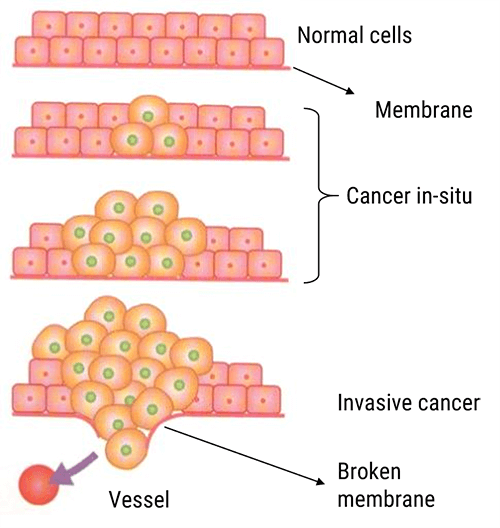
A normal cell becomes cancerous after important, progressive and irreversible modification.
Normal modifications are repaired by the body. However, when the cell becomes cancerous, it loses its ability to repair.
In a cancer, the cells undergo rapid multiplication, eventually forming a mass known as the malignant tumor.
These malignant tumors are named according to their cell type.
When the cancerous cells detach from the mother tumor, infiltrate in the blood or transplant on distant organs and then multiply on their own, this is referred to as metastasis.
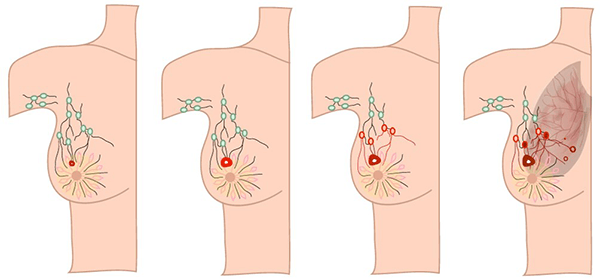
Breast cancer typically leave the breast through the lymphatic system. Most cancers travel to the lymph nodes in the axilla and from there to other parts of the body.
Some cancers will travel via the internal mammary nodes to the other breast.
In-Situ Carcinoma
Most cancers are slow growing and the initial stage of a cancer is called carcinoma in-situ meaning “remained in place”. In in-situ carcinomas there is no invasion to the neighboring tissues. If the tumor is not discovered at this stage, it will continue to enlarge and it will invade the surrounding tissues. At this stage it is called invasive cancer.
The mammogram plays a key role in the detection of in-situ ductal carcinoma. These cancers are generally non palpable and mainly identified by the appearance of microcalcifications.
- Comedocarcinomas which is very aggressive
- And non-comedomatous which is less progressive
Ductal Carcinoma In-Situ
Ductal Carcinoma In-Situ (DCIS) represents the proliferation of epithelial cells within the ducts. The cells are contained in the ductal, hence the name DCIS. In DCIS there is no break in the basement membrane and no connective tissue invasion.
Clinical Presentation
In the early stage these cancers are non-palpable mass. In the late stage a palpable mass can develop sometimes accompanied by nipple discharge if the cancer is growing in the large ducts behind the nipple.
DCIS represents 83% of all in situ cases of breast cancer diagnosed during 2010-2014.
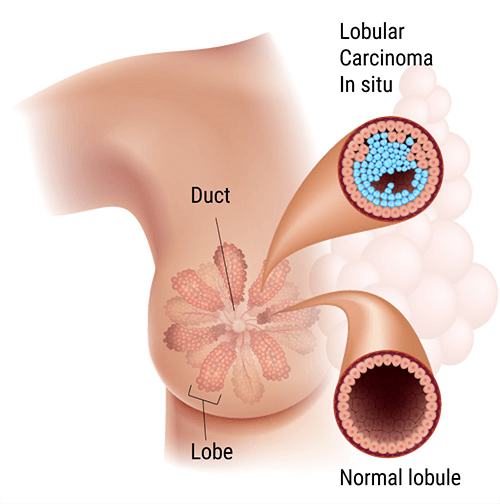
Lobular Carcinoma In-Situ
Another type of in-situ carcinoma is represented by proliferation of epithelial cells only inside the lobule. This is in-situ lobular carcinoma. In this cancer there is no break in the basement membrane or invasion of the cancer into the connective tissue. These cancers are not easily identified on the mammogram. They are often discovered accidently during biopsy of another abnormality.
In situ lobular carcinomas are often associated with lobular or ductal invasive carcinomas. They represent 12% of all in-situ breast cancers.
Invasive Carcinoma
If the cancer continues to grow, it is termed invasive. In infiltrating or invasive ductal carcinoma (IDC) there is proliferation of epithelial cells inside the ductal tree with basement membrane break and conjunctive tissue invasion.
In-situ cancers represents 20% of all breast cancers, while invasive cancers represent 80% of all breast cancers.
Infiltrating or invasive ductal carcinoma is often linked to high grade DCIS and is usually associated with a palpable mass.
On mammography this is seen as thin and polymorphous linear calcifications. There is segmental ductal distribution with or without a mass.
While on Ultrasound, these are seen as irregular shaped border masses. They are heterogenous echo-structures (invasive character).
The infiltrating or invasive lobular carcinoma (ILC) is represented by proliferation of epithelial cells outside the ductal units with break of the basement membrane and conjunctive tissue invasion. Invasive lobular cancer represents 10% to 15% of all invasive breast cancers. It is clinically and radiologically difficult to diagnose.
ILC is a cancer with slower evolution than ductal cancers, but offers a better prognosis if discovered early.
Metastasis is often spread out to the digestive tract and the ovaries. It is mostly bilateral. About 90% of these cancers are estrogen receptors positive, which means that they will respond to estrogen treatments. They are often associated with lobular carcinomas in-situ.
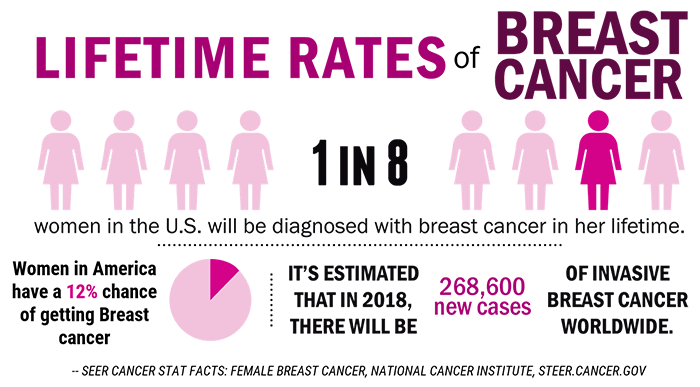
Incidence
Incidence in the United States
- 268,600 new cases of invasive breast cancer will be diagnosed in women in 2019
- 2,670 cases will be diagnosed in men
- And 62,930 cases of in-situ breast cancer will be diagnosed in women
During 2010-2014 the average age of occurrence was 62 years. In general, breast cancer risks and death rates will increase with age. Over the past 20 years the lifetime risk of a diagnosis of breast cancer has been increasing, mainly due to the longer life expectancy. However, beginning in 2000 the breast cancer incidence rates have begun to decline. This has been linked to the decrease used of hormone replacement therapy (HRT) by women.
Women in US have a 12.4%, or 1-in-8 lifetime risk of a diagnosis of breast cancer. While men on the other hand, have a 1-in-883 lifetime risk of diagnosis.
Breast cancer is the second most commonly diagnosed cancer in American women, right after Skin cancer which is the most commonly diagnosed.
Breast Cancer Mortality
Although the death rates have been decreasing since 1989, in 2019 about 41,760 women in the U.S. are expected to die from breast cancer.
Breast cancer survival varies with the stage at diagnosis and by tumor size.
- 99% for localized cases
- 85% for regional cases
- 27% for distant metastasis
Overall breast cancer death rates increased by 0.4% per year from 1975 to 1989. However, since 2015 there has been a rapid decrease in death rate from breast cancer. The decline averaging 39% through 2015.
Most of the decrease has been attributed to improved detection and treatment.
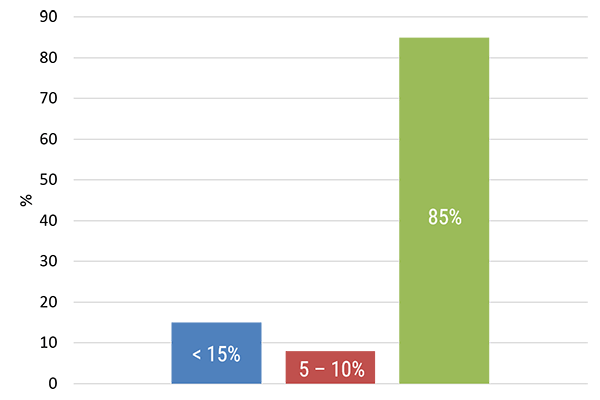
The most significant factor of breast cancer is gender (a woman) and age (growing old).
A woman’s breast cancer risks double if she has a first-degree relative (mother, sister, daughter) with a diagnose of breast cancer.
Less than 15% of women with breast cancer have a family member with a diagnose of breast cancer.
About 5-10% of breast cancers have a genetic link inherited from either mother or father.
About 85% of women with breast cancers have no family history of breast cancer.
In African-American women, breast cancer is common in women under 45. Also, African-American women are more likely to die of breast cancer often because of poor diagnosis and or treatment. Whereas, Asian, Hispanic, and Native-American women have a lower risk of developing and dying from breast cancer.
Knowing that breast density is an important factor in breast imaging, it is important to answer the following questions.
What is breast density? How does it affect breast cancer diagnosis? And what are the breast density reporting requirements?
As we mentioned earlier, breast tissues are composed of milk glands, milk ducts, supportive tissue (dense breast tissue), and fatty tissue (non-dense breast tissue).
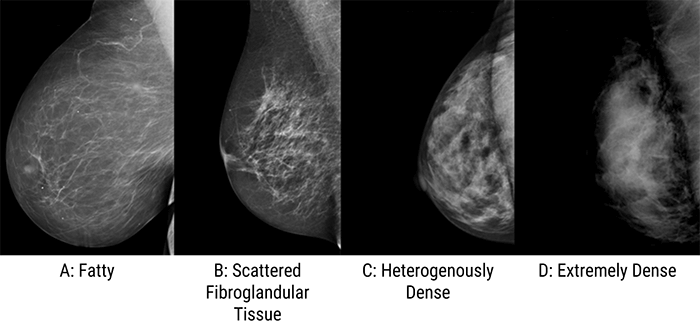
Breast tissue density defines the amount of fibrous and glandular tissue that appears on a woman’s mammogram.
Breasts are called “dense” when they are composed of more fibrous and glandular tissue than fatty tissue.
Please note that the glandular and fibrous breast tissue seen on a mammogram is white, while the fatty tissue appears dark. Therefore, the mammogram of a woman with dense breast tissue will appear whiter than that of a woman whose breast tissue is primarily fatty.
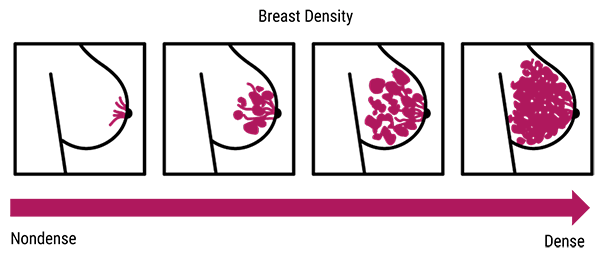
- Class A or level 1: In this case, the breast tissue is mainly composed of fatty tissue and contains less than 25% of glandular tissue
- Class B or level 2 where there are scattered areas of dense glandular and fibrous tissue, and the breast contains between 25-50% of glandular tissue
- Class C or level 3: in this case the breast is made of dense glandular and fibrous tissue (51-75%), described as heterogeneously dense)
- And finally class D or level 4 where breasts are extremely dense and composed of more than 75% glandular tissue
- Only 10% of women in the US have fatty breasts (Level 1)
- 40% of women have low level of density (Level 2)
- 40% of women have heterogeneously dense breasts (Level 3)
- And 10% have extremely dense breasts
While the American Cancer Society estimates that 40 to 50% of women who undergo a mammogram have heterogeneous or extremely dense breasts.
Breast density is often inherited, but some factors can also influence mammographic density levels.
Breast density may be influenced and affected by age, genetics, menopause, pregnancy, body weight and body mass index, use of alcohol and drugs such as tamoxifen.
Breast density decrease with age, pregnancy, higher body weight, menopause, and the use of tamoxifen.
Why the breast density and the distribution of glandular tissue within the breast are important, and how does breast tissue density affect a radiologist’s ability to detect breast cancer?
- First, an increased breast density is associated with reduced diagnostic accuracy
- Second, the amount of fibrous and glandular tissues within the breast is a predictor of future breast cancer risk, because when comparing women with extremely dense breasts to women with fatty breasts, the risk of developing breast cancer in women with dense breasts is increased by 4 to 6 times
- And third, for women with very dense breast tissue, other screening methods for detecting breast cancer may be recommended
As we all know, cancerous lumps and calcifications which may sometimes be associated with breast cancer, appear white on a mammogram, meaning that if the patient’s breast is dense, it will be harder to diagnose cancers.
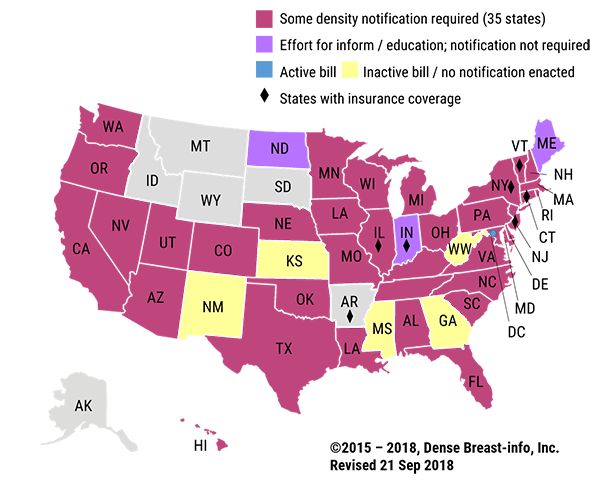
Breast Density Reporting Requirements
The Breast Density and Reporting Mammography Act of 2015 defines mammography facilities breast density reporting requirements that facilities must follow.
Mammography interpreters are now required to include information about breast density in both the summary of the written report that is given to the patient, and the final written report of mammography results that is sent to the physician.
- How breast density may mask cancer on a mammogram
- A qualitative assessment of breast density
- A reminder to individuals with dense breasts to discuss with their physician questions or concerns regarding the summary
As shown on this map, currently 38 states and the District of Columbia adopt this legislation. For further information please visit:
https://densebreast-info.org/legislation.aspx
Screening tests are used to find cancer before a person has any symptoms.
Therefore, let’s check now the American Cancer Society’s recommendations and guidelines for the early detection of breast cancer.
Because mammography can detect cancerous tumors which are not palpable and that patient would not notice during self-examination, and because early breast cancer detection leads to a greater range of treatment options, the American Cancer Society has set recommendations and guidelines for the early detection of breast cancer.
- Women ages 40 to 44 shall have the choice to start annual breast cancer screening with mammograms, if they wish to do so
- Women age 45 to 54 shall get mammograms yearly
- Women 55 and older shall switch to mammograms every 2 years, or can continue yearly screening
Screening shall continue as long as a woman is in good health and is expected to live 10 more years or longer, and all women shall be familiar with the known benefits, limitations, and potential harms linked to breast cancer screening.
Screening modalities
With the quick advancement of technology in the medical field, breast imaging and screening practices for breast cancer detection are changing.
Since 2000, around 96% of certified mammography facilities in the US use digital imaging units or what is known as full-field digital mammography (FFDM).
Some facilities have as well implemented digital breast tomosynthesis into their mammography screening routines.
Breast Computed Tomography is also a new imaging modality that provides three-dimensional (3D) images of the breast. It can be performed without breast compression and is not limited by breast density.
As you can see, different screening modalities and techniques are used for breast screening and cancer detection. Let’s detail each of these techniques and show their advantages and limitations especially when it comes to dose reduction.
Standard Mammography
- Analog mammography which is rarely used in today’s imaging world
- 2D Digital mammography which allows full digital technologies to be applied to mammography imaging
- And 3D Digital mammography or digital tomosynthesis
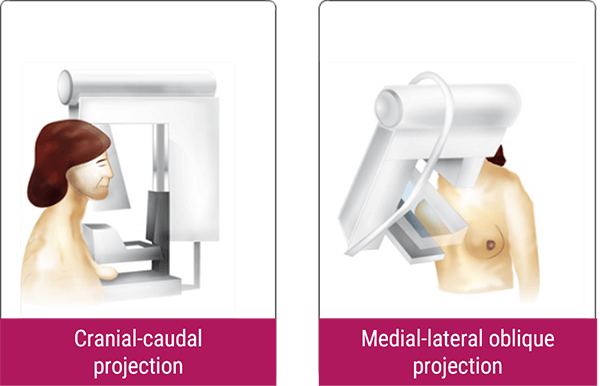
The patient positioning remains the same for all three technologies. And although the image acquisition changes for each technology, the basic structure of the x-ray tube design remains the same.
There are different types of detectors or image receptors divided between analog and digital imaging.
Over the years, mammography machines have changed greatly.
Analog mammography machines were the standard for many years. However, in 2000, the FDA approved the first full-field digital mammography unit, which improved image quality dramatically.
Analog mammography uses low dose radiation that produces high-quality X-rays and can detect tissue changes of 1-2mm in size. It captures the X-ray beams on film cassettes, and the outcome is a film showing the breast from different angles, which is then hung on a viewing board.
Contrary to this, digital mammography captures X-ray beams on a digital detector. This detector then converts the X-ray beams into electronic signals, which are transferred to a computer.
Actually, 2 types of Digital Systems exist:
The digital mammography using the indirect flat-panel techniques. And the Computed mammography based on the PSP technology: In PSP technology a cassette, called Image Plate (IP) is used with Photostimulable phosphor (PSP) technology. The IP is physically removed from the mammography unit and inserted into a computer Reader (CR) for processing.
Full-field digital imaging mammography refers to standard 2D digital imaging of the breasts.
- Ease of data sharing and storage
- Lower radiation exposure
- Improved contrast and magnification
- Quicker visibility of images
- Increased specificity
In addition, FFDM creates enhanced image contrasts with simple window leveling.
High contrast imaging is necessary to visualize the glandular versus fatty breast tissue and identify cancerous lesions.
And finally, patients tend to have less anxiety with digital mammography due to its ability to create images directly after the acquisition.
- Standard projections are inadequate
- A suspicious area is seen on one projection only
- And a suspicious area needs work-up to avoid the trauma of surgery
Projections can also be added to the imaging series by the technologist when the standard projections do not image all breast tissue. For example if there is extra breast tissue in the lateral aspect of the breast that is not covered on the routine CC, an XCCL may be added to the imaging series. We will cover the supplementary projections later.
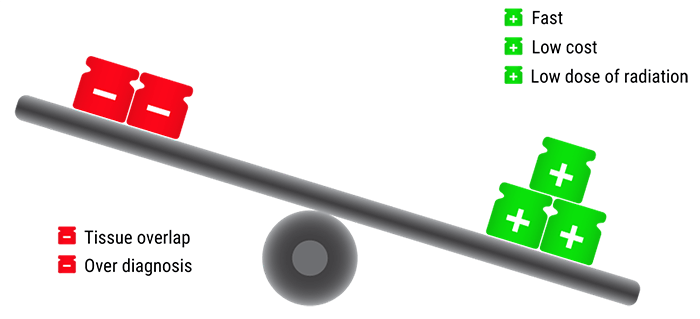
As a summary, standard mammography, including FFDM and film screen, is a fast, low cost, noninvasive X-ray technique that emits a low dose of radiation. However, when the breast is compressed, breast tissues may overlap. This overlapping can cause the resulting image to look like cancer.
In addition, in standard mammography 20 to 30% of breast cancers may be missed by the radiologist due to tissue overlap.
Standard mammography can also lead to over diagnosis, which is the screen detection of breast cancers that would not cause any harm to a patient in their lifetime and would likely not been detected in the absence of screening.
Despite these limitations, standard mammography remains the best tool and the most effective method of early breast cancer detection.
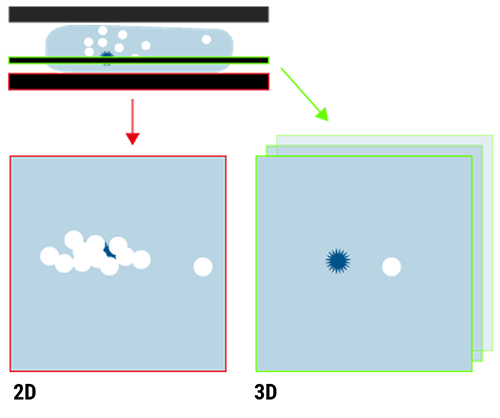
It is well known that full-field 2D digital mammography is limited by tissue superimposition. Overlapping tissue can mask tumors resulting in a false negative result and mimic tumors resulting in a false positive result.
Digital Breast Tomosynthesis
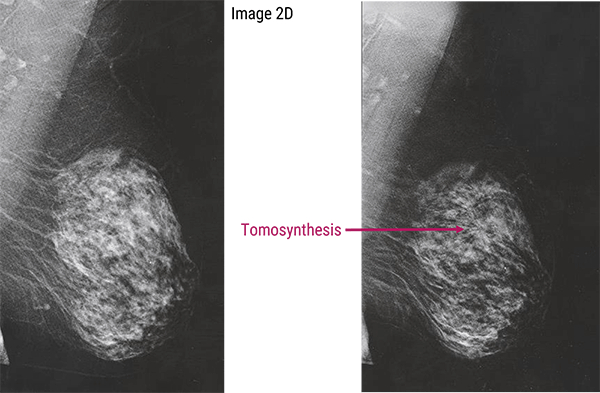
That’s why the digital breast tomosynthesis was introduced. This new technology can help improve the radiologist’s ability to diagnose breast cancer, since it is a three-dimensional imaging technique that images the breast in layers and decreases the superposition of normal tissues.
On February 2011, the US Food and Drug Administration (FDA) approved the use of DBT system in combination with 2D mammography for breast cancer imaging.
In digital breast tomosynthesis, the x-ray tube moves in a limited arc angle while the breast is compressed and a series of exposures are obtained.
Low-dose full field projection images of the breast are obtained from different angles. Each projection image requires only a fraction of the total dose of a full 2D mammogram. The images are then reconstructed in 3D volume. The number of reconstruction images will be based on the breast thickness in mm. Typically, the number of images acquired ranges from approximately 10 to 25 depending on the mammography unit. The angle ranges from about 10 to 50°.
It is important to note that DBT can be performed at approximately the same total radiation dose used for 2D mammography.
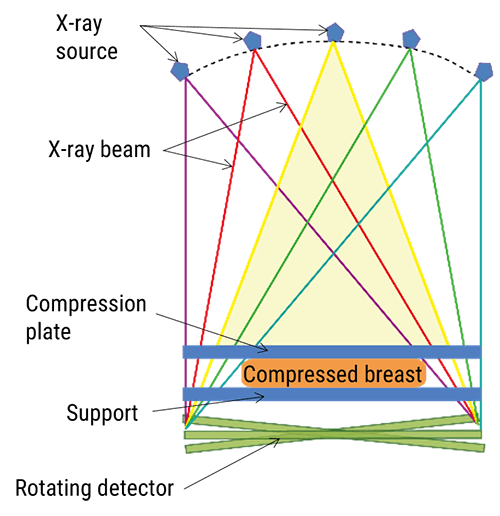
In DBT imaging, structures located at different depths will project at different locations.
A sequence of projection images are acquired. These projections are reconstructed in 3D volume and into 1 mm slices.
The angle of the tube travel and the number of acquired images depends on the manufacturer, slice thickness, and thickness of the breast.
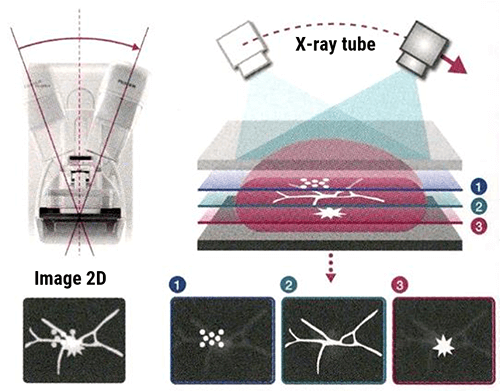
Advantages of digital breast tomosynthesis include: Reduction of the recall rate, increased breast cancer detection rate since benign lesions are seen clearly and overlapping structures are eliminated. In other words, the superposition of tissues in the 2D mammography that can hide lesions (left image), are eliminated in the DBT mode.
However, Digital breast tomosynthesis (DBT) has a few minor drawbacks: It acquires a large number of images, motion artifacts are hard to detect at the radiologist workstation in some DBT units, there is significant increase in reading time, and increased possibility of motion because of the longer exposure time.
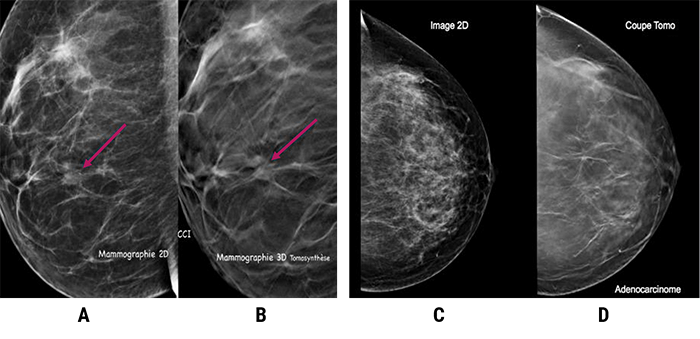
These images show the advantage of 3D.
In image A, a lesion that is indistinct is clearly seen on the 3D in image B.
In the image C, the dense parenchyma of the breast hides the microcalcifications seen in image D.
The areas of stellate lesion (arrow) is seen clearly on the 3D on the right. In the 2D image, the dense parenchyma of the breast hides this lesion.
Breast Computed Tomography
To overcome the loss of information that occurs in 2D screening, in addition to DBT, Breast Computed Tomography (BCT) was also introduced. BCT is a diagnostic tool that produces 3D images with high symmetric resolution of the breasts.
Breast computed tomography uses a wider arc than DBT and produces more images.
With this technology multiplanar image reconstructions such as sagittal and coronal projections may be created from the original transverse image sets.
In dedicated BCT, 300 to 500 low-dose projections are acquired following a circular trajectory around the breast.
This technology can be used for the evaluation of suspicious features such as microcalcifications, masses and asymmetries.
However, Breast Computed Tomography has limited ability to detect small objects such as small calcifications.
It is currently used as a supplemental tool in diagnostic accuracy and is not being considered yet as a screening mammography tool.
In screening mammography, radiation exposure to a patient can be expressed in different ways including absorbed dose, entrance or skin dose, mean glandular dose, and bone marrow dose.
It is important to understand which method of measuring radiation dose to the breast is most often employed.
Absorbed Dose
When X-rays pass through the breast or any other body part, some but not all will interact with the atoms of the patient’s body.
When the incident photon interacts with an electron and gives all its energy to the electron, the photon disappears and its energy is transferred to an electron. This action is called absorption.
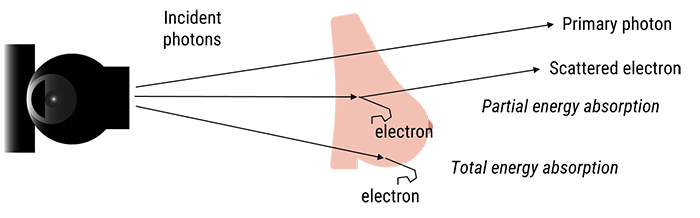
The amount of energy absorbed per unit mass is known as the absorbed dose. It is the amount of energy deposited within the tissue being radiated, and is expressed in Gray which is equivalent to Joules/kg.
The greater the amount of energy that passes through the body, the greater the possibility of producing biological damage to the patient. However, without this process and the differences in the absorption properties of different body structures, it would not be possible to produce diagnostically significant images.
Entrance Skin Dose
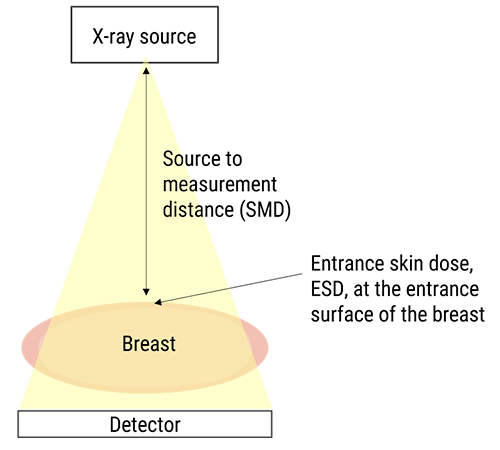
In general to measure the amount of radiation received by a patient, radiological exposures with human phantoms are conducted. Therefore, for breast imaging, breast phantoms are used.
The entrance skin dose is the measure of the radiation dose that is absorbed by the skin as it reaches the patient. Entrance skin dose is measured by placing a dosimeter on the patient’s skin or on top of a phantom.
ESD is considered as a poor indication of radiation risk because it does not take into consideration the tissue sensitivity, the penetration and the area of the x-ray beam.
Besides, you shall always remember that mammography screening should not be compared to conventional radiology because the energy of X-rays applied during a mammography examination is lower than the X-ray energy used while imaging other parts of the body, this is due to the molecular composition of the breast.
Second, in mammography screening, the field of view is restricted only to the breast and its surrounding tissues. And third, the frequency of mammography imaging is higher when compared to other imaging exams because of breast cancer screening recommendations.
Moreover, there are variances amongst patients that we should take into consideration. These variances include differences in breast densities, age, and risk factors.
For example, women aged between 45 and 54 will receive more breast exposure when compared to women above 54 or under 45.
In addition, following breast cancer screening recommendations, women who are at high risk of developing breast cancer will undergo more mammography examinations and thus will receive more breast exposure in their lifetime.
The type of imaging technique used during mammography also affects the amount of breast radiation exposure.
Mean Glandular Dose
As we mentioned earlier, entrance skin dose is not that relevant, therefore the mean glandular dose was introduced in the late 1980s.
Besides, breast glandular tissue presents a high risk of developing cancer, this is why in mammography screening, the radiation dose deposited in the glandular tissue is of greater concern, and the measurement of the glandular dose (Dg) is most often used.
Mean glandular dose (MGD) is the main descriptor of absorbed dose to the breast.
It varies in a very complicated way, with differences noted in X-ray beam quantity and quality (kV and mA).
Glandular dose is approximately 15% of the Entrance Skin Dose (ESD), and can be calculated using this equation: MGD = Dg x ESD where Dg is the glandular dose and ESD is the Entrance Skin Dose
- The characteristics of the equipment used
- The examination technique
- Breast density, thickness, and shape
- And the X-ray beam

Monte Carlo Techniques
Monte Carlo techniques are sophisticated techniques used to physically measure the radiation dose to the breast. They are the principal tool for dosimetry in screening mammography.
These techniques are based on computer simulations of the X-ray beam passing through a well-defined breast phantom to quantify the energy deposited in the glandular tissue.
The conversion coefficients used for mammography are called the normalized glandular dose. They are the ratio of the absorbed dose in the glandular tissue divided by the entrance surface of the breast and the free-in-air kerma at the center of the field of view.
In this last section, we will discuss and compare the radiation dose levels with each of the previously listed techniques.
Screening Mammography
As mentioned previously, modern mammography machines use very low dose radiation, therefore the risk of harm is minimal.
On average the total dose of a typical mammogram with 2 projections of each breast is about 0.4 millisieverts.
People in the US are normally exposed to an average of 3 mSv of radiation each year from their natural surroundings. Therefore, the dose of radiation used for a screening mammogram of both breasts is equal to the amount of radiation a woman would get from her natural surroundings over 7 weeks.
Digital and Analog Mammography
Over the years, mammography machines have changed greatly.
Analog mammography machines were the standard for many years. However, in 2000, the FDA approved the first full-field digital mammography unit, which improved image quality dramatically.
When compared to traditional screen film mammography, FFDM offers better contrast and lower spatial resolution at a lower radiation dose.
Studies have shown that full-field digital mammography had 22% lower mean glandular dose than screen-film mammography per view.
DBT
The first DBT unit was approved by the FDA in November 2011.
Digital breast tomosynthesis is a form of limited angle tomography. In DBT, multiple low dose images of the breast are taken from different angles. A study completed in 2017 comparing the radiation dose received from DBT to the dose received from FFDM showed the following:
For skin entrance dose, DBT had lower mean dosage compared with full-field digital mammography, and mean glandular doses for both breasts were lower in DBT compared with FFDM. Which means that DBT showed lower mean glandular dose and entrance dose compared with FFDM.
Digital Breast CT
Breast computed tomography (DBCT) is a new imaging modality that provides three-dimensional images of the breast. It can be performed without breast compression and is not limited by breast implants or breast density.
It is a supplemental examination used to follow-up on suspicious lesions or for women who have been diagnosed with breast cancer.
Dedicated breast CT received US Food and Drug Administration approval for diagnostic use in 2015. And recent studies have shown that the radiation dose level of DBCT is similar to the dose of FFDM.
Over the past 10 years, various methods of breast imaging have been introduced.
FFDM, DBT, and CBT have been approved by the FDA for breast screening with demonstrated success in dose reduction.
DBT and CBT can provide valuable information in the third dimension and can overcome the issue of tissue overlap, allowing better detection of malignant tumors.
On the other hand, breast density has become an important part of preventive breast care, and physicians are now required to notify patients whether or not they have dense breasts. This allows the patient with dense breasts to seek appropriate breast imaging and ensure proper health.
Finally, ACR recommendations shall be followed to decrease mortality from breast cancer.
Post-Test & CE Certificate:
Add to CartPrice: $6.00
| ✔ | Approved by the ASRT (American Society of Radiologic Technologists) for 1.5 Category A CE Credits |
| ✔ | License duration: 6 months from purchase date |
| ✔ | Meets the CE requirements of the following states: California, Texas, Florida, Kentucky, Massachusetts, and New Mexico |
| ✔ | Accepted by the Nuclear Medicine Technology Certification Board (NMTCB) |
| ✔ | Meets the ARRT® CE reporting requirements |
As per the ARRT regulations, you have up to 3 attempts to pass the Post-Test with a minimum score of 75%.
Upon the successful completion of the Post-Test (score 75% or more), you will need to fill up a 1 min survey and then you will be able to issue your CE Certificate immediately.
Refund Policy: Non-Refundable


